Session Information
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Rheumatic disease (RD) patients are at increased risk for prosthetic joint infections (PJI), however, diagnosis is challenging because active RD may mimic joint infection and definitive microbiologic diagnosis may be delayed. We aimed to identify the clinical and microbiological features of total hip (THA) and total knee arthroplasty (TKA) PJI in RD and OA patients, using an institutional PJI registry and compare the incidence of culture negative (CN) PJI in RD vs OA. Baseline clinical differences between CN-RD and culture positive (CP)-RD and OA PJI as well as the relationship of infection free survivorship of the prosthesis were also evaluated.
Methods: A retrospective cohort of THA/TKA PJIs, from 2009 to 2016, were identified by ICD codes, and confirmed by chart review. RD cases were also confirmed by use of RD-specific medications. CN cases were defined as PJIs with no evidence of microbial growth in intraoperative cultures and CP PJI cases were defined by positive microbial growth in intraoperative cultures. Treatment failure was defined as subsequent surgical treatment for infection after the index procedure- debridement, antibiotics and implant retention (DAIR), one stage or two stage exchange. Demographics, medications, microbiology, surgical therapy and outcome were abstracted. Baseline characteristics were evaluated using Fisher’s exact and Chi-Square tests.Kaplan-Meier estimates were used to calculate infection free survivorship.
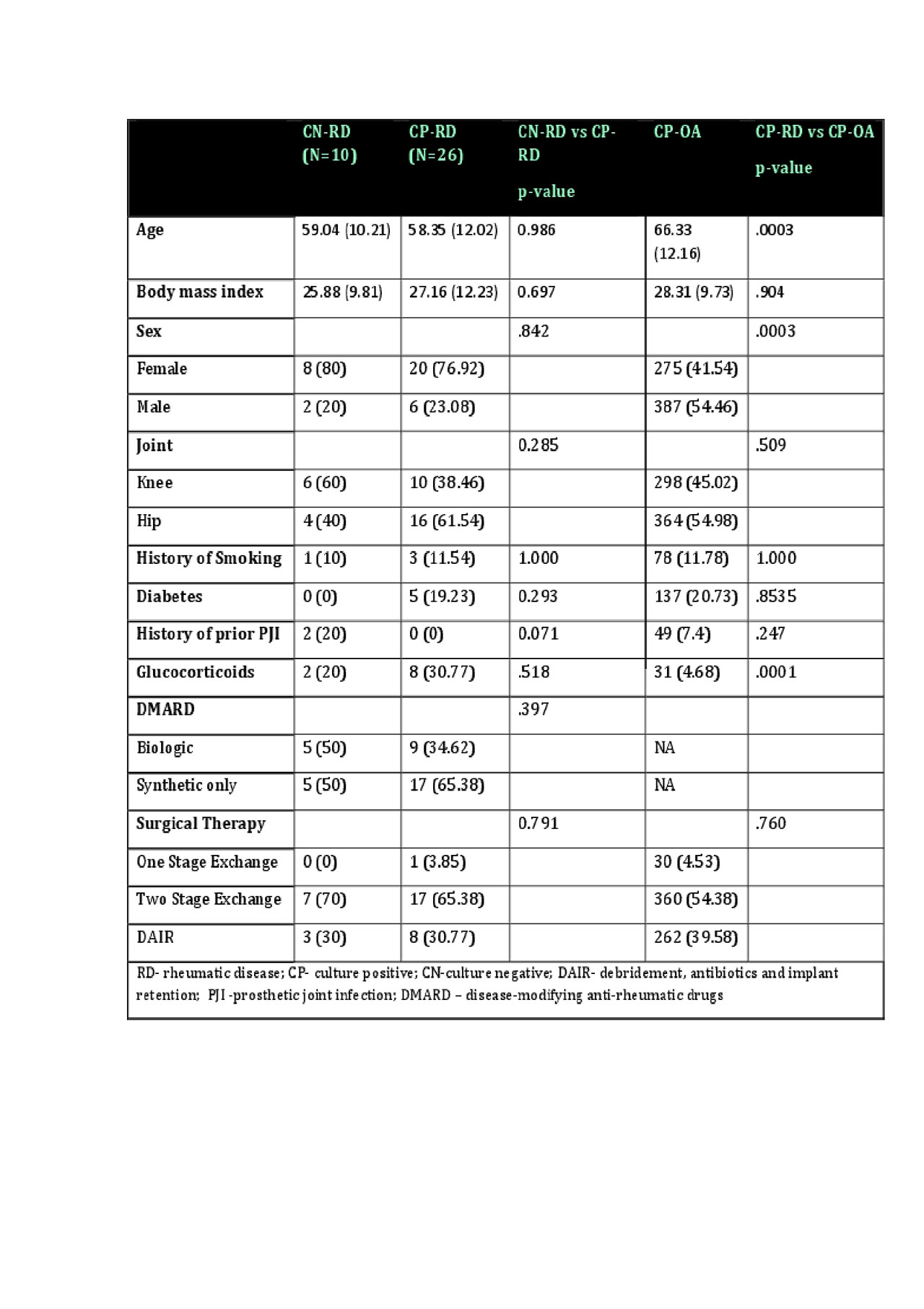
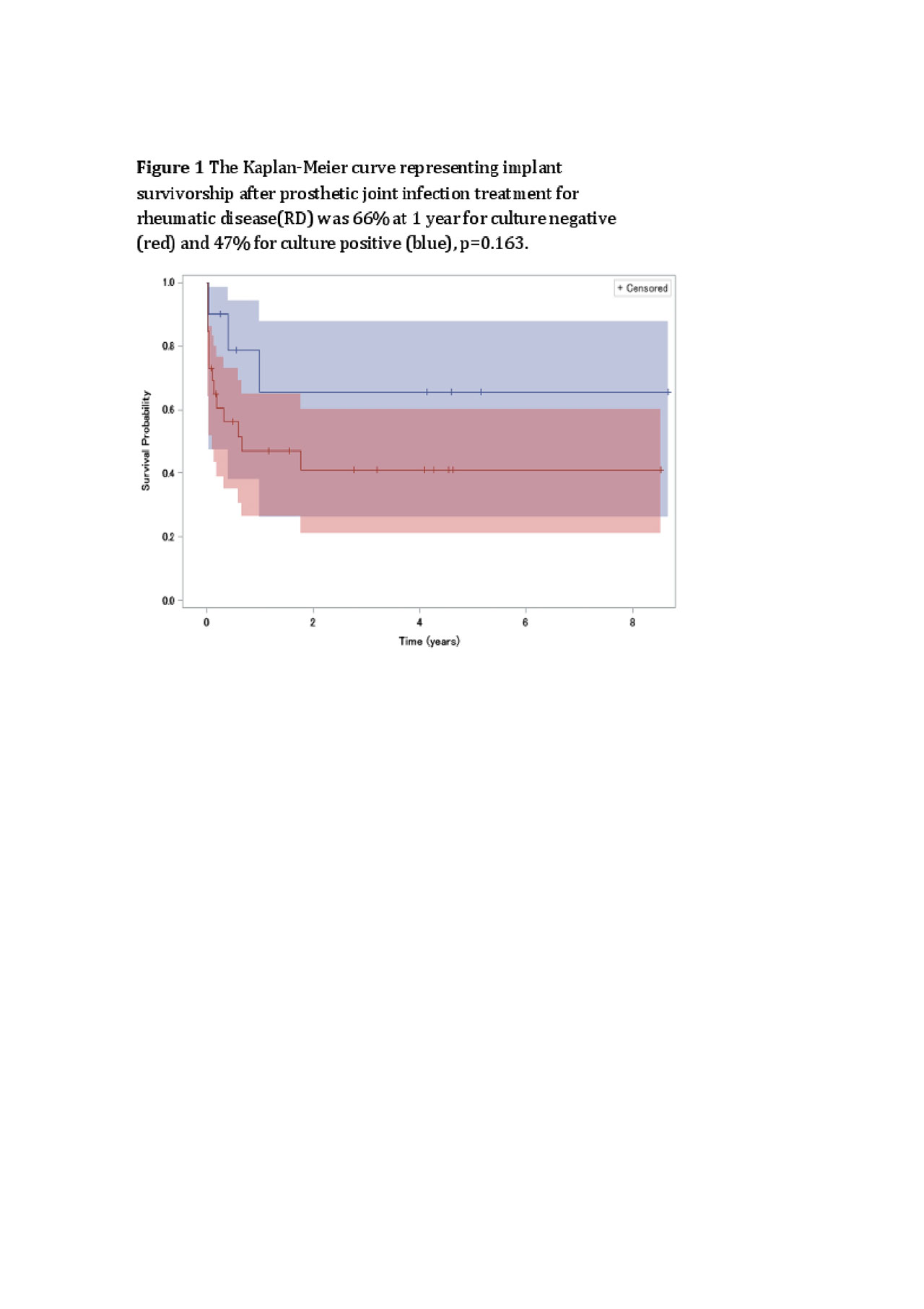
Results: 807 PJI cases were identified including 36 RD (33 RAand 3 SLE) and 771 OA. A higher proportion of RD PJI were CN (N=10, 27%) vs. OA PJI (N=109, 14%, p=0.02). Fewer CN-RD cases met PJI histopathology criteria compared to CN-OA, (p=0.08). On average, RD-CN were younger than OA-CN (59 vs 69, p=.01), but no different than RD-CP cases. One year survivorship of CN-OA and CN-RD were 87% and 66%, respectively and 47% for CP-RD. Comparing CN-RD vs. CP-RD, no difference was observed in age, smoking, diabetes, or Charlson comorbidities, but a trend towards higher prevalence of prior PJI in the CN-RD group. No differences were found in surgical treatment (p=0.92) or use of biologics and DMARDs (p=0.12) between CN and CP RD patients. Among CP cases, there was no difference in diabetes, comorbidities, smoking, or history of PJI, but more RD were female (p=.0003) and used glucocorticoids (p=.0001). Across all CP cases, 57.4% were Staphylococcal, with no differences between groups. Overall surgical treatment included 2-stage exchange (54.8%), DAIR (39.24%) and 1-stage exchange (4.51%), with no differencebetween groups (p=0.76). Treatment failure was more frequent for CP-RD (30.4% vs 42.3%), but the difference was not significant (p=0.19).
Conclusion: RD PJIs are more likely to be culture negative than OA PJIs, but small numbers limit our analysis. Prior PJI, histopathology and better outcomes suggest biologic differences between CN and CP PJI that should be explored further.
To cite this abstract in AMA style:
Goodman S, Kapadia M, Miller A, Donlin L, Henry M, Russell L, Figgie M, Nocon A, Sculco P. Clinical Features of Prosthetic Joint Infections in Patients with Rheumatic Diseases vs Osteoarthritis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/clinical-features-of-prosthetic-joint-infections-in-patients-with-rheumatic-diseases-vs-osteoarthritis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-features-of-prosthetic-joint-infections-in-patients-with-rheumatic-diseases-vs-osteoarthritis/