Session Information
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Familial Mediterranean fever (FMF) is an auto-inflammatory disease characterized by recurrent episodes of fever and polyserositis. Most patients have their first febrile attack before the age of 20. Elderly onset (after 40 years) is very rare, but we do encounter these patients sometimes. Therefore, the aim of this study was to evaluate the demographic, clinical, and genetic characteristics of late-onset FMF patients in the Japanese population.
Methods: We analyzed clinical features and mutations in the MEFV gene of 384 patients, who were referred to our laboratory (Department of Medicine [Neurology and Rheumatology], Shinshu University School of Medicine) between September 2003 and September 2016. All patients were clinically diagnosed with FMF by the Tel-Hashomer criteria. Patients were divided into three groups based on the age of disease onset; group I: 19 years and younger (early-onset group), group II: 20–39 years, group III: 40 years and older (late-onset group). Mutation analysis of the MEFV gene was performed by direct sequencing of the product of polymerase chain reaction amplification for hotspot regions (exons 1, 2, 3, 5, and 10). Differences between categorical variables were analyzed using chi-square test with Bonferroni correction. Continuous variables were evaluated with Kruskal-Wallis test and multiple comparison.
Results: The study enrolled 63 patients (16.4%) who experienced their first FMF attack when older than 40 years. In this patient group, high fever (90.5%) was the most common clinical finding. In contrast, the percentage of patients with peritonitis (66.2% in group I, 66.8% in group II, 34.9% in group III) and pleuritis (47.0% in group I, 36.5% in group II, 27.0% in group III) was significantly lower in late-onset patients compared with early-onset patients. In the late-onset group, the frequency of patients having a mutation in the MEFV gene (57.1%) and a mutation in exon 10 (12.7%), which induces a severe clinical FMF phenotype, was significantly lower than in early-onset patients. The response to colchicine therapy was good (88.6%) and similar in all groups. Family history of FMF was less frequent in the late-onset group.
Conclusion: In Japan, there are a number of FMF patients with late-onset. Our observation indicates that they have a milder form of the disease with less frequent peritonitis and pleuritis and a good response to colchicine treatment. However, careful differential diagnosis may be needed because they have a lower prevalence of the MEFV gene mutation, especially in exon 10.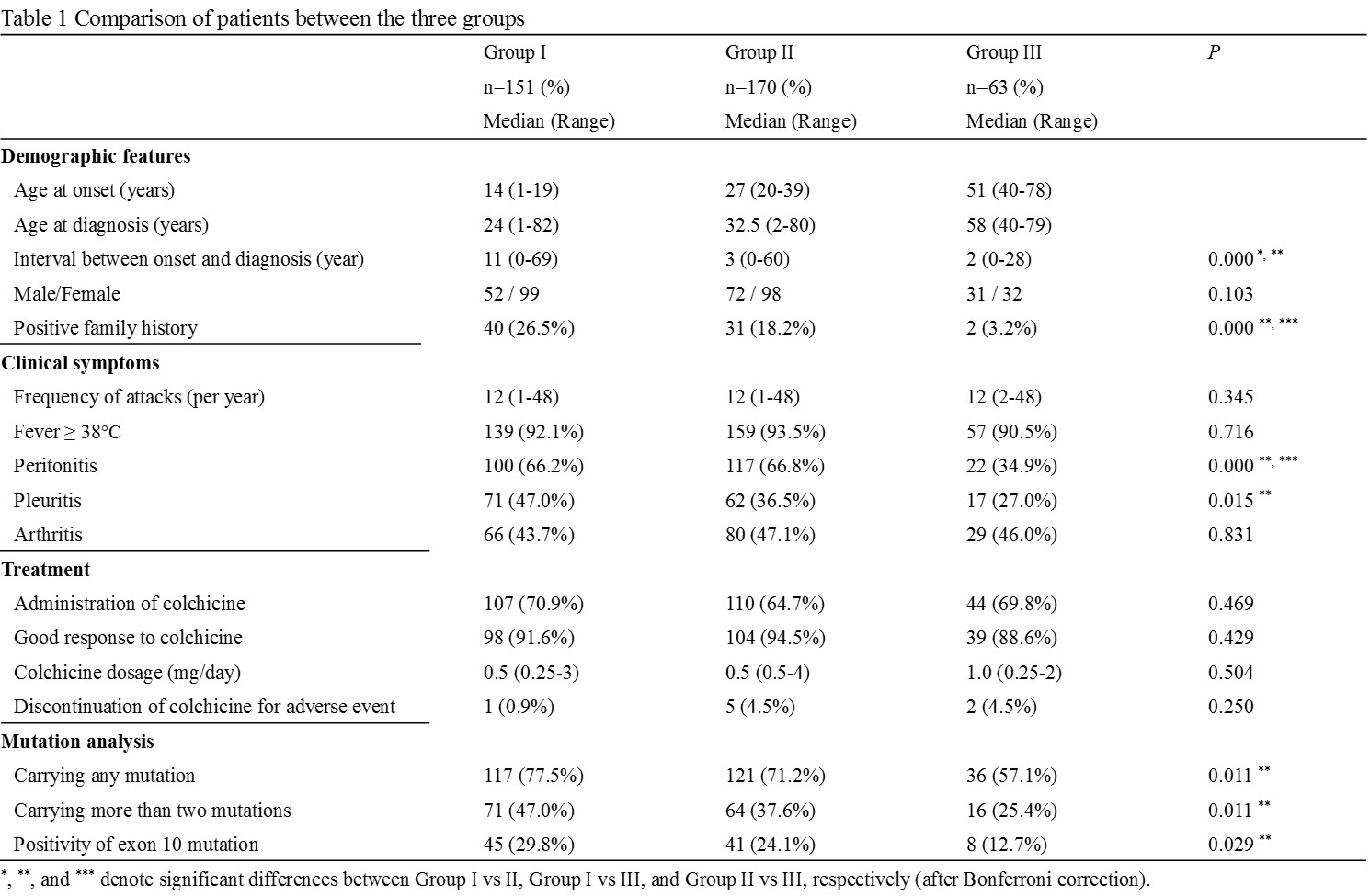
To cite this abstract in AMA style:
Kishida D, Yazaki M, Nakamura A, Tsuchiya-Suzuki A, Shimojima Y, Sekijima Y. Clinical Characteristics of Patients with Late-Onset Familial Mediterranean Fever in Japan [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/clinical-characteristics-of-patients-with-late-onset-familial-mediterranean-fever-in-japan/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-characteristics-of-patients-with-late-onset-familial-mediterranean-fever-in-japan/
