Session Information
Date: Saturday, November 12, 2022
Title: Vasculitis – ANCA-Associated Poster I: Epidemiology, Outcomes, and Classification
Session Type: Poster Session A
Session Time: 1:00PM-3:00PM
Background/Purpose: ANCA-associated vasculitides (AAV) induced by anti-thyroid drugs (ATD) is a well-known entity. However, characteristics, requirement for immunosuppressive agents and the risk of relapse remain poorly studied. We aimed to describe the clinical characteristics and outcome of patients with ATD-induced AAV in comparison to primary AAV.
Methods: We performed a retrospective multicenter study of patients with ATD-induced. ATD-induced AAV were defined as the development of AAV after ATD initiation until one year after ATD discontinuation. Patients were classified as granulomatosis with polyangiitis (GPA), microscopic polyangiitis (MPA) or eosinophilic granulomatosis with polyangiitis (EGPA) according to 2022 ACR/EULAR classification criteria. We further focused on MPA patients and compared patients with ATD-induced MPA and those with primary MPA. Each ATD-induced MPA was matched with 4 primary MPA on gender and year of diagnosis. Baseline characteristics and treatments were compared with t-tests for continuous variables, and chi-2 tests for categorical variables. Remission-free-survivals were compared with Cox proportional hazard ratios models, adjusted on age at MPA diagnosis and on renal involvement.
Results: Forty-six patients with ATD-induced AAV were included. Twenty-eight (60%) fulfilled criteria for MPA, 8 (17%) criteria for GPA, one (2%) criteria for EGPA, and nine (19%) patients had unclassified AAV. Among the 46 patients, 97% were ANCA-positive, including MPO-ANCA in 22 (47%), PR3-ANCA in 6 (13%), and both MPO- and PR3-ANCA in 15 (32%). Main clinical manifestations were skin (65%), arthralgia (52%), and glomerulonephritis (34%).. At diagnosis, 1966 Five Factor Score was 0 for 81%, 1 for 4% and 2 for 15% of the patients.Therapeutic management was based on ATD discontinuation in 97% of cases, allowing vasculitis remission in 17%. Eighty-three percent of patients required an induction regimen including glucocorticoids in 100%, in combination with rituximab in 30% and cyclophosphamide in 19%. Maintenance therapy was initiated in 91% of the patients, mainly based on glucocorticoids. Anti-thyroid drugs were reintroduced in 8 cases (17%) and patients did not experience any relapse.
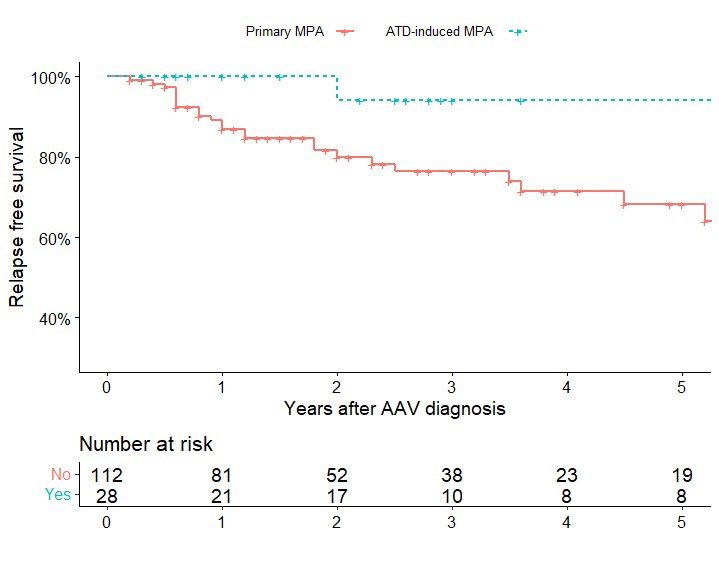
Patients with ATD-induced MPA (n=28) were compared with 112 matched primary MPA. Compared with primary MPA, ATD-induced MPA were significantly younger at diagnosis (49 vs. 65 years, P< 0.001), had less frequent renal involvement (43 vs. 76%, P=0.02), but more frequently cutaneous (53 vs. 25%, P=0.007) and ocular involvement (14.3 vs. 2.7%, P=0.042). ATD-induced MPA had a lower mean BVAS (9.9 vs. 13.1, P=0.023) at diagnosis. Finally, the risk of relapse was lower in ATD-induced MPA than in primary MPA (adjusted HR 0.07; 95%CI 0.01-0.62, P=0.016) (Figure).
Conclusion: In this multicenter retrospective cohort, ATD-induced AAV were mainly MPA with MPO-ANCA, but double MPO- and PR3-ANCA positivity was frequent. ATD-induced MPA were less severe and showed a lower risk of relapse than primary MPA.
To cite this abstract in AMA style:
Culerrier J, Nguyen Y, Karadag O, Bilge S, DEMIRCI YILDIRIM T, Öğüt T, Yazisiz V, Bes C, Cefle A, Sadioglu Cagdas O, Yazici A, Kronbichler A, Jayne D, Regent A, Teixeira V, Marchand-Adam S, Duffau P, Oro S, Andre B, Luca L, Lechtman S, Aouba A, Lebas C, Servettaz A, Dernoncourt A, Ruivard M, Milesi A, Poindron V, Jego P, Padoan R, Delvino P, Vandergheynst F, Pagnoux C, Yacyshyn E, Lamprecht P, Flossmann O, Puéchal X, Terrier B. Clinical Characteristics and Outcome of ANCA-Associated Vasculitides Induced by Anti-Thyroid Drugs: A Multicenter Retrospective Cohort Study [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/clinical-characteristics-and-outcome-of-anca-associated-vasculitides-induced-by-anti-thyroid-drugs-a-multicenter-retrospective-cohort-study/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-characteristics-and-outcome-of-anca-associated-vasculitides-induced-by-anti-thyroid-drugs-a-multicenter-retrospective-cohort-study/