Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: anti Jo-1 antibodies are the main marker of the antisynthetase syndrome (As), a connective tissue disease chiefly characterized by arthritis (A), myositis (M) and interstitial lung disease (I). These manifestations may occur concomitantly but incomplete clinical pictures have been described. Aim of this study is to further characterize clinical presentation and course of anti Jo-1 positive As
Methods: data from multicentre, multinational series of patients diagnosed with anti Jo-1 positive As were retrospectively collected and analyzed. Anti Jo-1 antibodies were tested in all cases by commercially available ELISA techniques
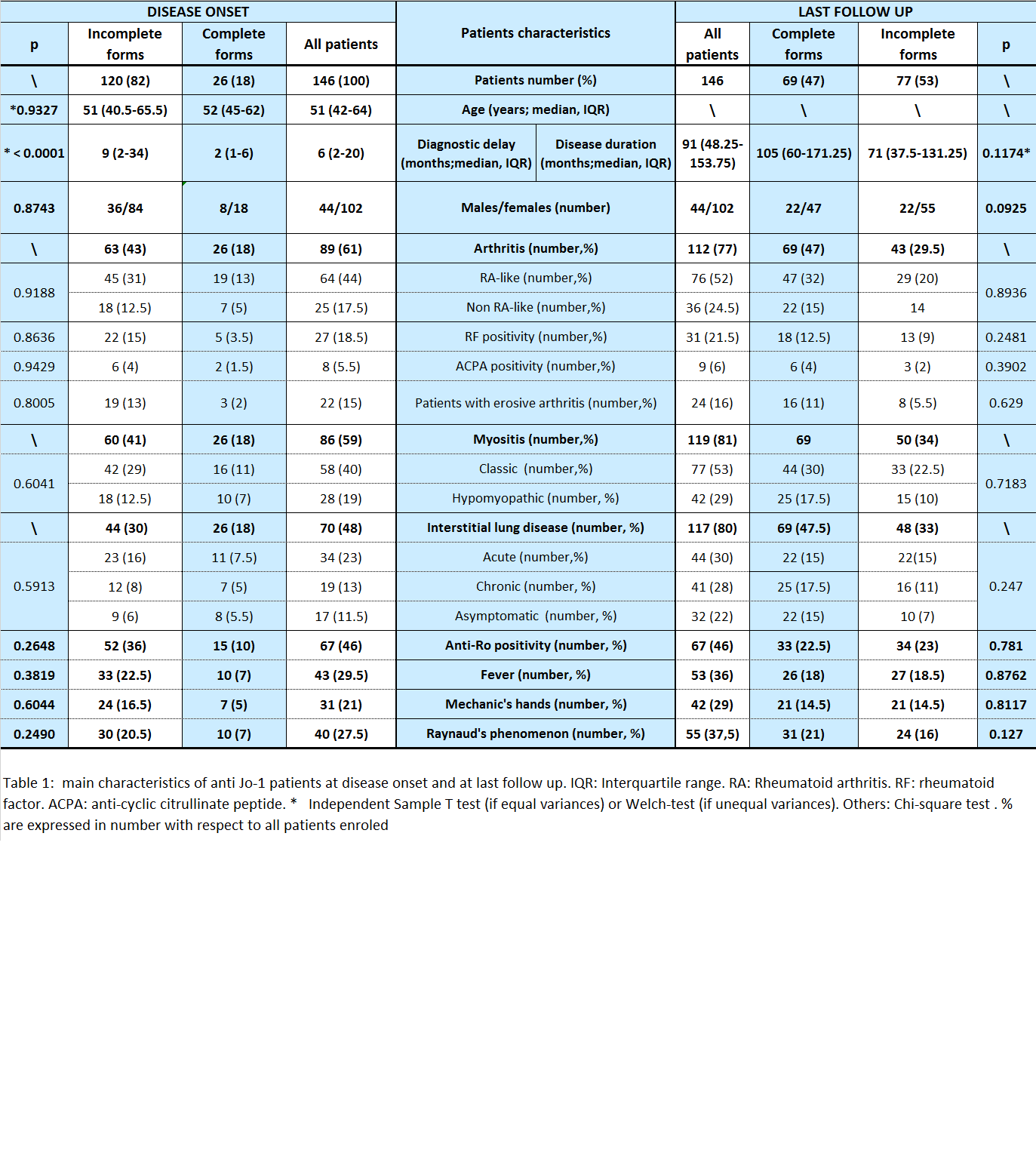
Results: 146 patients were included (Table 1). Median follow up was 91 months (IQR 40.25-153.75). At the onset, a complete clinical picture (AMI) was present in 26 patients (18%). Seventy-two patients (49%) had monosymptomatic presentation (A 36, 24.5%; M 20, 14%; I 16, 11%), 19 AM (13.5%), 19 MI (13.5%) and 10 AI (7%). Arthritis was the most frequent feature at the onset, the only detectable in 24.5% of patients. Many patients meet the 2010 ACR/EULAR classification criteria for rheumatoid arthritis (RA). Rheumatoid factor, anti citrullinated peptide antibodies and RA typical radiographic erosions were not a rare finding. Time from clinical onset to diagnosis was longer in incomplete forms (p<0.001). During the follow up, 69 patients (57.5%) developed additional features (median time to progression: 17 months, IQR 7.5-43.5). Progression rate was significantly higher in patients with single feature onset (57/72) with respect to those with two features (12/48) (p<0.001). At the last follow-up, 69 patients (47%) had AMI, 23 (15.5%) AM, 23 (15.5%) MI, 16 (11%) AI, 8 (5.5%) I, 4 (3%) A and 3 (2%) M. Twenty-five patients (17.5%) died, 7 (5%) due to As progression. First line treatment was based on corticosteroids (140 patients, 96%) and immunosuppressants (112, 77%; hydroxychloroquine, HCQ, 30; methotrexate, MTX, 24; IV cyclophosphamide, CYC, 20; cyclosporine, Cys, 20; azathioprine, AZA, 17; mycophenolate mofetil, MMF, 4; tacrolimus, TC, 3; other not listed). Globally, MTX was prescribed in 58 patients (40%, 22 withdrawn for side effects/ineffectiveness), Cys in 47 (32%, 10), AZA 36 (24.5%, 21), CYC 34 (23%, 23), HCQ 34 (23%, 21), MMF in 17 (11.5%, in 5), TC in 9 (6%, 5)
Conclusion: the diagnosis of anti Jo1 positive As may be delayed in incomplete forms, which are the vast majority at presentation. Joint involvement may be very similar to RA, adding further challenges to differential diagnosis. Clinical picture evolution is common in patients presenting with incomplete forms and it may occur even after several years from disease onset. Treatment appears heterogeneous and with high drop-out rates in both first and second line. This suggests the need of better strategies supported by specific recommendations
Disclosure:
L. Cavagna,
None;
M. A. González-Gay,
None;
S. Castañeda-Sanz,
None;
F. Franceschini,
None;
P. Airo,
None;
I. Cavazzana,
None;
L. Nuno,
None;
T. Pina Murcia,
None;
F. J. Lopez Longo,
None;
N. Ortego-Centeno,
None;
R. Neri,
None;
S. Barsotti,
None;
E. Fusaro,
None;
S. Parisi,
None;
G. Paolazzi,
None;
G. Barausse,
None;
L. Quartuccio,
None;
E. Bartoloni-Bocci,
None;
C. Selmi,
None;
C. A. Scirè,
None;
E. Bravi,
None;
J. Bachiller Corral,
None;
L. A. Saketkoo,
None;
G. Bajocchi,
None;
R. Pellerito,
None;
M. Govoni,
None;
A. Schwarting,
None;
C. Specker,
None;
C. Montecucco,
None;
R. Caporali,
None.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-and-temporal-characterization-of-anti-jo-1-positive-anti-synthetase-syndrome-preliminary-results-of-an-international-multicentre-study/