Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Antiphospholipid syndrome (APS) is closely linked with Systemic Lupus erythematosus (SLE) and can influence patient outcomes. The interplay between APS and SLE, including the evolution of one condition into the other, remains an area of significant clinical interest. This study aims to evaluate the duration and frequency of evolving APS in SLE patients and vice versa and identify clinical and serological predictors for each condition’s progression to the other.
Methods: A retrospective cohort study was conducted across three tertiary hospitals in Saudi Arabia. A diagnosis with Primary APS and a diagnosis with SLE who met the included criteria were recruited, aged more than 16, were first diagnosed in the hospital with at least one clinic visit per year, and did not have any other autoimmune disease overlap or other thrombophilia. Clinical data, laboratory results, and patient demographics were analyzed to assess the frequency, duration, and risk stratification associated with each disease progression.
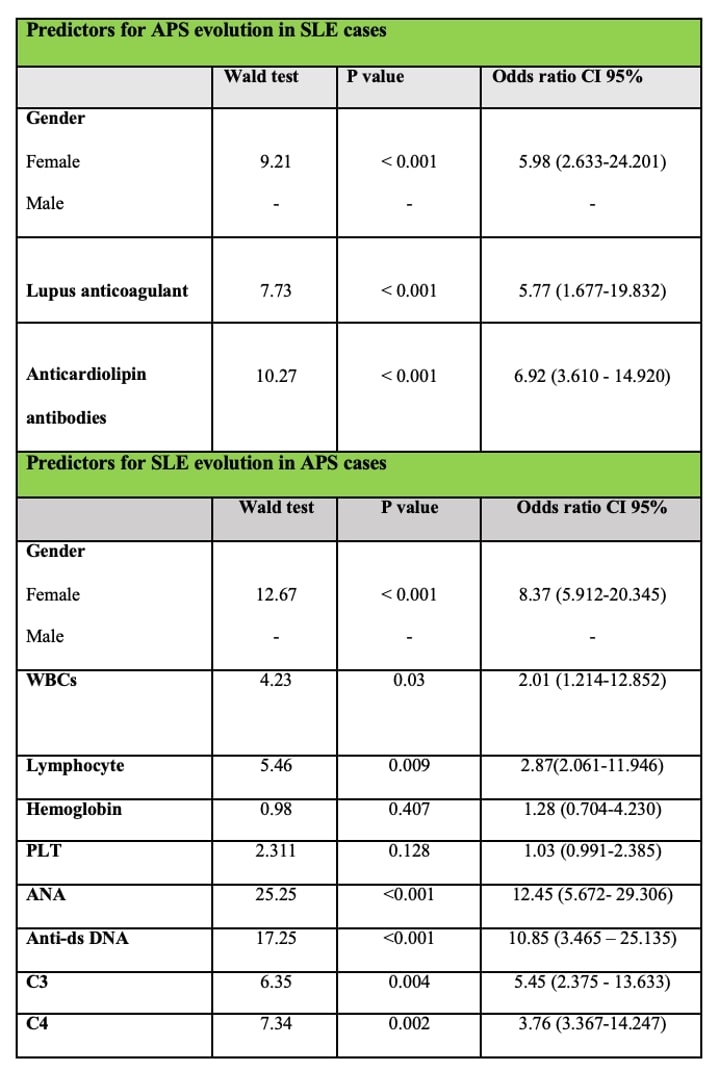
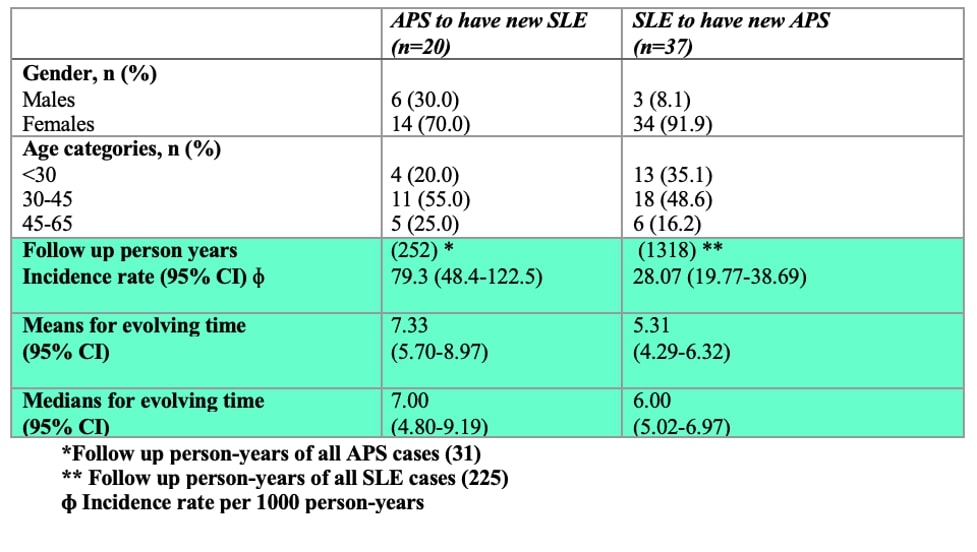
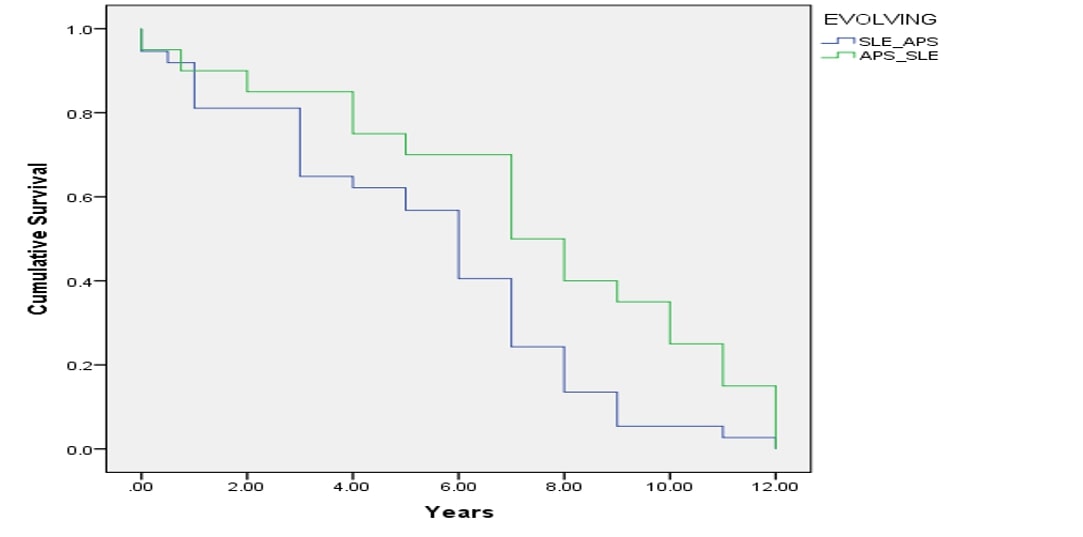
Results: A total of 256 patients, diagnosed with (225) SLE and (31) diagnosed as primary APS, were included. APS patients had a higher mean age at diagnosis (34.35 ± 9.76 years) compared to SLE patients (29.36 ± 11.73 years) (p=0.009). APS patients showed lower frequencies of constitutional symptoms, cutaneous manifestations, and musculoskeletal involvement compared to SLE patients. Significant predictors for APS evolution in SLE patients included female gender [OR 5.98 (2.633-24.201)], Lupus anticoagulant [OR 5.77 (1.677-19.832)], and anticardiolipin antibodies [OR 6.92 (3.610 – 14.920)]. For SLE evolution predictors in APS patients were female gender [OR 8.37 (5.912-20.345)], low WBC counts [OR 2.01 (1.214-12.852)], low lymphocytic count [OR 2.87(2.061-11.946)] positive ANA [OR 12.45 (5.672- 29.306)], positive Anti-DsDNA [OR 10.85 (3.465 – 25.135)], low C3 [OR 5.45 (2.375 – 13.633)], and low C4 [OR 3.76 (3.367-14.247)] levels (Table 1). Table 2 highlights the higher incidence rate of having new SLE cases in APS patients (79.3 per 1000 person-years) compared to new APS cases in SLE patients (28.07 per 1000 person-years). The Kaplan-Meier curve showed in patients diagnosed with APS, the mean time to develop new SLE cases is 7.33 years (95% CI: 5.70-8.97), with a median time of 7 years (95% CI: 4.80-9.19). However, for patients diagnosed with SLE, the mean time to develop new APS cases is 5.31 years (95% CI: 4.29-6.32), with a median time of 6 years (95% CI: 5.02-6.97) (Figure 1).
Conclusion: The incidence rates of evolving APS in SLE patients and vice versa highlight the dynamic nature of these autoimmune conditions. These findings underline the critical importance of vigilant monitoring and timely intervention by rheumatologists in patients with primary APS to facilitate early SLE detection, similarly, anticipation of APS should be emphasized for patients with SLE, focusing on the identified risk factors of the progression of one condition into the other.
To cite this abstract in AMA style:
Elnady B, Alakkas Z, Abdulaziz S, Halabi H, A. G. Ibrahim A, Draz H, Attar M, Daghasi H, Alhalwani A, Shaker R, Maher Elsheikh G. Clinical and Serological Distinctions and Evolutionary Predictors in Antiphospholipid Syndrome and Systemic Lupus Erythematosus: A Multicenter Cohort Analysis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/clinical-and-serological-distinctions-and-evolutionary-predictors-in-antiphospholipid-syndrome-and-systemic-lupus-erythematosus-a-multicenter-cohort-analysis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-and-serological-distinctions-and-evolutionary-predictors-in-antiphospholipid-syndrome-and-systemic-lupus-erythematosus-a-multicenter-cohort-analysis/