Session Information
Date: Sunday, November 13, 2022
Title: Osteoporosis and Metabolic Bone Disease – Basic and Clinical Science Poster
Session Type: Poster Session C
Session Time: 1:00PM-3:00PM
Background/Purpose: Fractures in patients with systemic lupus erythematosus (SLE) are more common than age and sex matched controls. Fracture risk is traditionally assessed by dual-energy X-ray absorptiometry (DEXA) measured BMD and refined using the Fracture Risk Assessment Tool (FRAX). Several studies have demonstrated fractures in SLE patients despite normal DEXA BMD. We hypothesize that changes in bone microarchitecture may explain fracture vulnerability in SLE. This study was initiated to characterize bone quality by evaluating measures of microarchitecture at the proximal femur via 3T MRI in patients with SLE and compare these measurements with a control group of patients with known low bone density (LBD) and osteoporosis (OP).
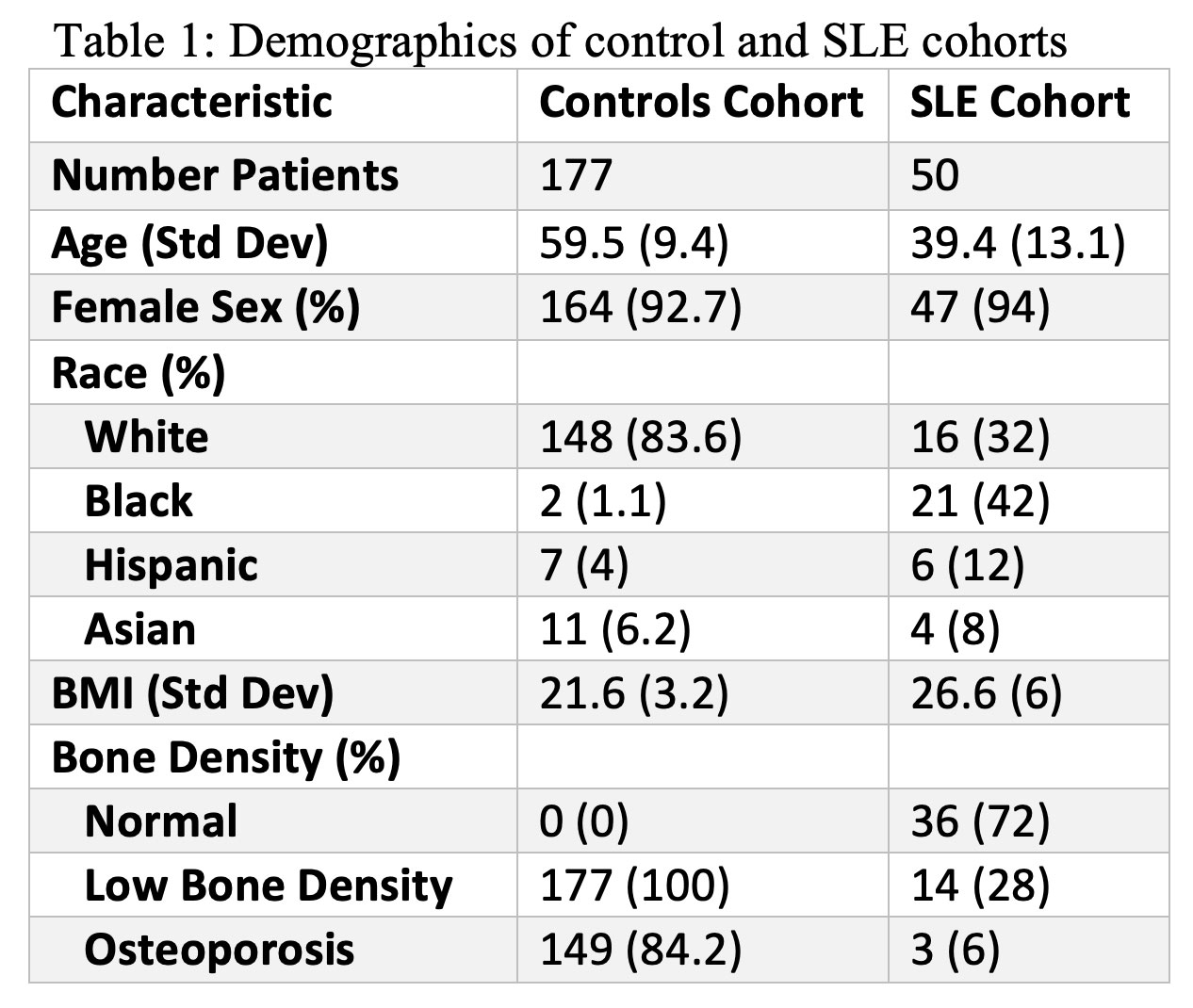
Methods: 50 SLE patients and 177 controls with known LBD or OP underwent DEXA and 3T MRI of the non-dominant hip. DEXA measured BMD of the total hip, femoral neck, and spine. LBD was defined as Z score ≤ -2.0 in premenopausal women and men younger than fifty, and T score ≤ -1.0 in others. OP was defined as the presence of LBD and history of fragility fracture in premenopausal women and men younger than fifty, and T score ≤ -2.5 in others. MRI measured favorable microarchitectural characteristics trabecular plate width (PW), trabecular plate-to-rod ratio (PRR), plate volume fraction (PVF), trabecular bone thickness (Tb.Th), and trabecular network area (NA), as well as unfavorable characteristics rod volume fraction (RVF) and trabecular spacing (Tb.Sp). Demographics, medication use and inflammatory markers at the time of the study visit were recorded. Statistical analysis was performed using Pearson correlations, t-scores, and multivariable linear regressions as appropriate.
Results: 50 SLE patients and 177 patients with LBD or OP completed all imaging studies. The SLE cohort was younger, and a higher percent of black patients compared to controls (Table 1). SLE patients had lower MRI PW and PRR and higher Tb.Sp as compared to controls, while having higher DEXA BMDs at all sites after adjustment for confounders (Figure 1). SLE patients had an inverse relationship between ESR and PW, PRR, Tb.Th, and NA (Figure 2, A-D). Similar results were found with CRP, which had an inverse relationship with PW, PRR, and NA. Body mass index (BMI) in SLE patients had an inverse relationship between PW, PVF, Tb.Th, and NA (Figure 2, E-H), and a positive relationship between all measured BMDs. In the control group, similar relationships were found between BMI and BMD, but only Tb.Th was inversely associated with BMI. Age, current steroid use, and history of lupus nephritis were not associated with MRI measures of bone microarchitecture.
Conclusion: Compared to controls, SLE patients had decreased bone quality as measured by MRI bone microarchitecture, despite having higher DEXA BMD. Elevated inflammatory markers inversely associated with bone quality. Elevated BMI, despite its association with higher BMD, was also associated with lower measures of bone microarchitectural strength, unlike controls. Further connection of bone microarchitecture to fracture risk and change over time in patients with SLE are needed to determine clinical significance of these findings and to guide additional monitoring and potential treatments.
To cite this abstract in AMA style:
Novack J, Chang G, Honig S, Monga A, Zhang X, Saha P, Martel D, Izmirly P, Belmont H, Buyon J, Saxena A. Characterizing Bone Microarchitecture with MRI in Patients with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/characterizing-bone-microarchitecture-with-mri-in-patients-with-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/characterizing-bone-microarchitecture-with-mri-in-patients-with-systemic-lupus-erythematosus/