Session Information
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Pain control in rheumatic diseases is complex
and various pharmacotherapy approaches can be utilized for management of
rheumatic pain. Currently, systematic clinical practice guidelines for pain
management in Rheumatoid Arthritis (RA) are lacking; however, there are several
evidence-based expert recommendations provided by a broad panel of
rheumatologists from the 3e initiative1. Based on these
recommendations, the aim of this study was to describe patient-reported
pharmacotherapy regimens involved in the management of rheumatic pain in early
vs. established RA.
Methods: Patient-reported medication data was collected from
the Ontario Best Practices Research Initiative (OBRI), a clinical cohort of RA
patients followed in routine care. As recommended by the 3e initiative,
patients receiving NSAIDs, acetaminophen (APAP), opioids, antidepressants (AD)
and neuromodulators (NM) at cohort-entry or while in the OBRI were selected (n
= 1,470) and followed till a change in pain therapy was reported. Based on
disease duration, patients were categorized into early RA (disease duration ≤1
year) or established RA (disease duration >1 year). For each group, patient
demographics, common pharmacotherapy regimens and the number of patients
receiving each regimen were determined.
Results: From the selected cohort, 384 patients met the
criteria for early RA and 1,054 patients for established RA. 32 patients did
not indicate their disease duration and were excluded. In early RA, the mean age
± SD of patients was 56.4±14.2 years, 73.2% were female and mean disease
duration ± SD was 0.42±0.49 years. In established RA, the mean age ± SD of
patients was 57.4±12.0 years, 80.0% were female and mean disease duration ± SD
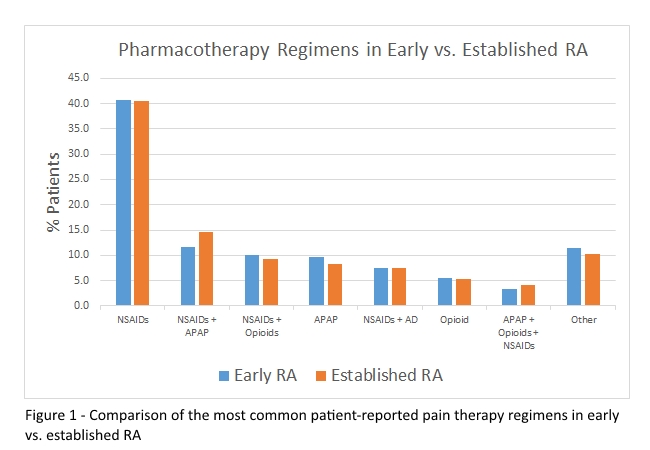
was 11.9±9.41 years. The most common pharmacotherapy regimens and % patients
receiving each regimen are shown in figure 1.
Conclusion: Our study showed that NSAID use as monotherapy
or in combination with other agents was highly prevalent across both groups.
Patients with established disease were more likely to use a combination of NSAIDs
+ APAP and NSAIDs + opioids + APAP possibly due to worsening pain with disease
progression. The use of NSAIDs + opioids was higher in early RA. Physicians may
feel more comfortable prescribing opioids in early RA due to the advent of
Ontario’s Narcotic Monitoring System as well as better patient education and
follow-up with dedicated pain clinics. Further work is required to determine
the association between pain therapy regimens and disease activity measures in
early vs. established RA.
References
1. Whittle SL, Colebatch AN, Buchbinder R, Edwards CJ, Adams K,
Englbrecht M et al. Multinational evidence-based recommendations for pain
management by pharmacotherapy in inflammatory arthritis: integrating systematic
literature research and expert opinion of a broad panel of rheumatologists in
the 3e initiative.Rheumatology2012;51:1416-25.
To cite this abstract in AMA style:
Kelkar A, Cesta A, Li X, Bombardier C. Characterization of Patient Reported Pain Medication in Early Vs. Established Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/characterization-of-patient-reported-pain-medication-in-early-vs-established-rheumatoid-arthritis/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/characterization-of-patient-reported-pain-medication-in-early-vs-established-rheumatoid-arthritis/