Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Thrombocytopenia has been reported at frequencies ranging from 10 to 40 % in different cohorts. Treatment can be challenging and due to its considerable impact on prognosis, it has been of important concern. We aimed to identify clinical and laboratory characteristics, and prognosis of SLE patients with thrombocytopenia in a large single centre cohort.
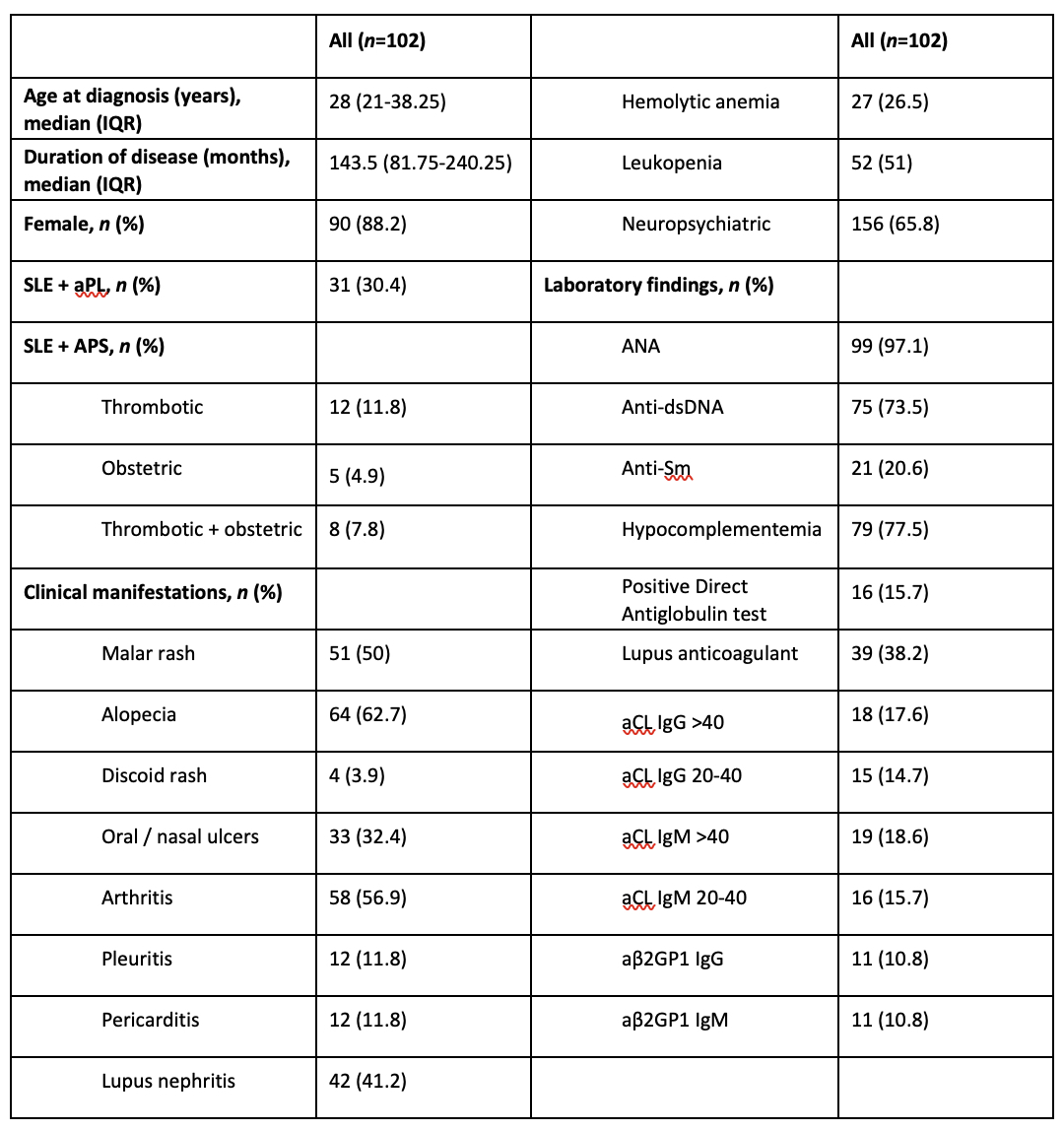
Methods: The study included 102 patients with chronic ( >12 months) or acute (< 3 months) thrombocytopenia. Data regarding clinical and laboratory characteristics, disease duration, treatments and responses, disease activity (SLEDAI) and damage (SLICC/ACR SDI), and bleeding history were retrieved from the database and revised. Thrombocytopenia was defined as a platelet count of < 100 × 109/L and was confirmed by a peripheral blood smear. “Early”, “initial”, and “durable” treatment responses were defined as a platelet count of >30 × 109/L and at least doubling baseline at first week, first month and 6th month, respectively. Remission was defined as a platelet count of >100 × 109/L 12 months after treatment. Relapse was defined as a platelet count of < 100× 109/L or a >50% decrease in a patient in remission.
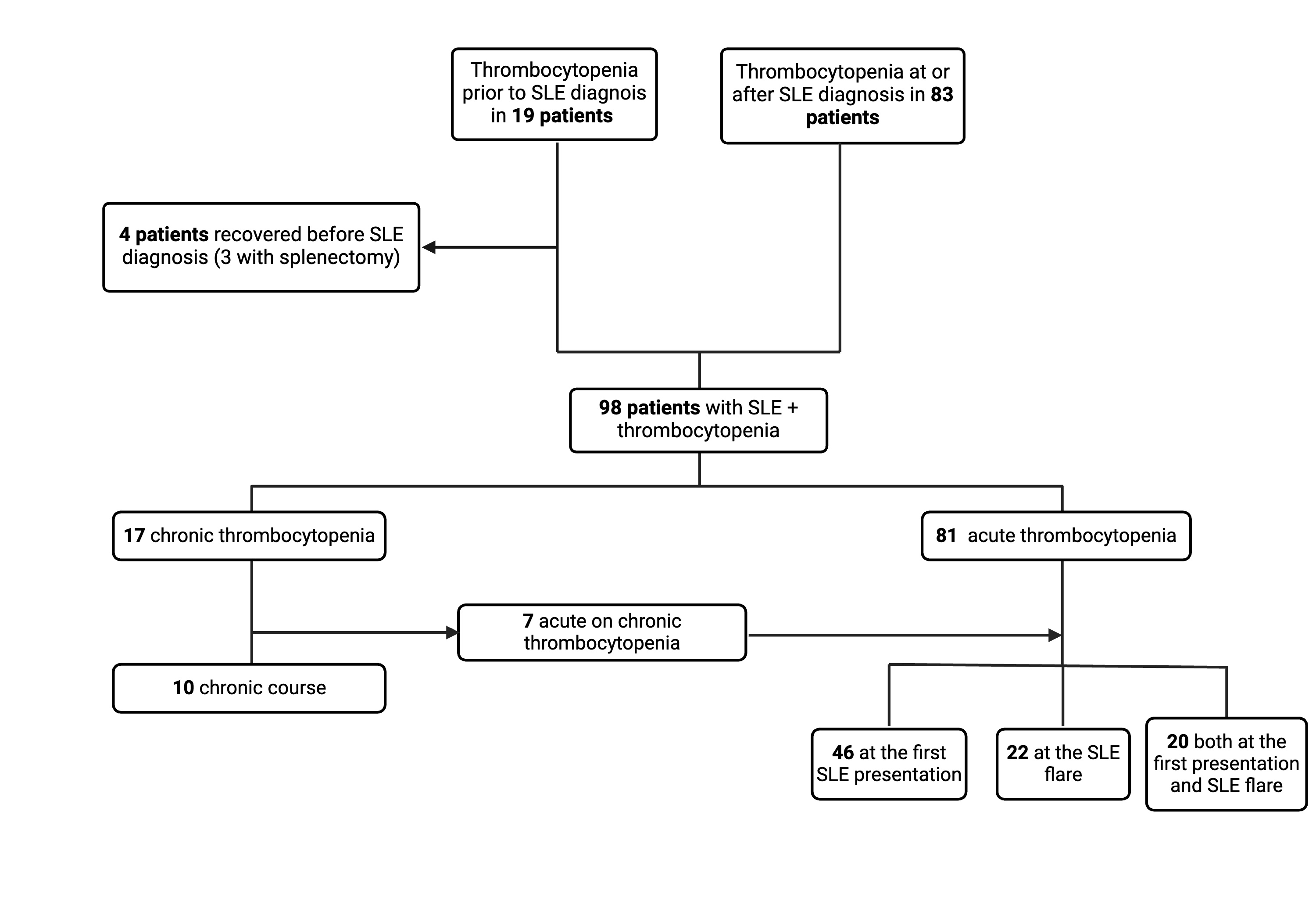
Results: Of 102 patients (characteristics shown in Table 1), 83 were diagnosed at the time of SLE diagnosis or during the course, and 19 prior to diagnosis. As 4 of the latter (3 with splenectomy) did not relapse after SLE diagnosis, they were excluded from the analysis (Figure 1). Mean SLEDAI of 66 patients with acute thrombocytopenia at SLE diagnosis was 16.8 (± 9.9), and 40 (60.2%) had a SLEDAI >12. Platelet count was ≤20 × 109/L in 17 patients (25.7%) and >50 × 109/L in 30 (45.5%). Sixty-five patients (98.5%) were managed with glucocorticoids, initiated with intravenous pulse in 32 (48.5%). IVIG was required in 4 (6.1%) patients, CYC was used in 20 (30.3%), AZA in 29 (43.9%) and MMF in 9 (13.6%). Early response was achieved in 21 (31.8%) patients, initial response in 50 (75.8%), and durable response in 60 (90.9%). There was at least one relapse in 38 patients. Among immunosuppressives, only CYC was found to reduce the risk of relapse (relapse rate: 10% vs 39.1%, P=0.021). Early response did not reduce the risk of relapse. At the first relapse, rituximab was administered to 9 of 25 patients, and 7 of them did not relapse again. Total 5 patients underwent splenectomy due to refractory disease and 4 of them had no further relapse. Binary logistic regression analysis showed that aPL positivity was a risk factor for relapse [OR (95% CI): 3.8 (1.4-10.3), P=0.009]. Minor bleeding occurred in 24 patients and major bleeding in 13. Median SDI was 1 (IQR:0-3) and 65 patients (63.7%) had SDI ≥1. Patients with at least one relapse had a higher SDI than those with no relapse (mean SDI: 2.7 (± 2.4) vs 1.4 (±2.0), P=0.008).
Conclusion: Thrombocytopenia may precede SLE, can be detected at the time of diagnosis or during the course of the disease. Patients with aPL positivity have higher risk for relapse. Since relapse is associated with higher damage, prevention is important. First-line CYC treatment was associated with a low risk of relapse. Rituximab, which has been shown to be effective in relapses, can be considered as first-line treatment whilst splenectomy may be considered in refractory cases.
To cite this abstract in AMA style:
Uludag O, Aghamuradov S, Erel Gezegen C, Jabbarli M, Habibov I, Celik A, Yalcinkaya Y, Gul A, Inanc M, Artim Esen B. Characteristics, Treatment Responses and Prognosis in a Single Center Cohort of SLE Patients with Thrombocytopenia [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/characteristics-treatment-responses-and-prognosis-in-a-single-center-cohort-of-sle-patients-with-thrombocytopenia/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/characteristics-treatment-responses-and-prognosis-in-a-single-center-cohort-of-sle-patients-with-thrombocytopenia/