Session Information
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Psoriasis (Pso) is one of the most common chronic inflammatory skin diseases in Europe. Psoriatic arthritis (PsA) is closely associated to Pso whereas the skin manifestation appears usually years before PsA-related symptoms emerge. Up to 30% of Pso patients develop PsA, but there is no clear correlation between disease duration of Pso and PsA development. Therefore, biomarkers for its early detection are of major importance. In early PsA, changes in synovial vascularisation combined with increased expression of proangiogenic factors appear first. Therefore, imaging biomarkers for detection of changes in vascularisation can be useful for early detection of joint disease. Fluorescence-optical imaging (FOI) is a new method to detect changes in microvascularisation of the hands.
Methods: Sensitivity of FOI for detection of subclinical signs of inflammation as biomarker for early PsA was observed in a prospective, multicentre study (XCITING) including patients with dermatological confirmed skin psoriasis only. 411 patients were included from dermatology care units across Germany without diagnosis of PsA but potential risk factors for its development (nail psoriasis and/or joint pain or swelling within the last 6 months). Clinical examination (CE; swollen (66) and tender (68) joint count, enthesitis, dactylitis assessment) and standardised ultrasound (US) assessment was performed by a qualified rheumatologist to assess musculoskeletal inflammation. FOI was performed additionally. Data was analysed in focus on increased vascularisation of musculoskeletal structures of both hands as inflammatory marker. In cases of discrepant results (positive FOI and negative results for CE and US), MRI was performed to prove the findings.
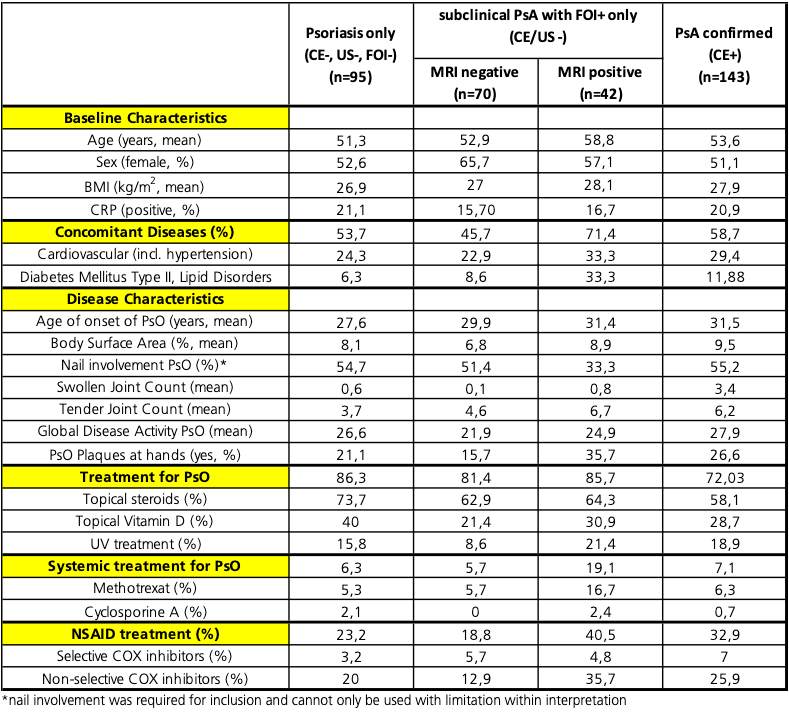
Results: 83 of the 411 patients of the cohort were negative in all assessments (Pso only). 112 patients showed subclinical signs of musculoskeletal inflammation in the central reading of FOI, whereas CE and US were negative. In 37,5% of those patients, subclinical inflammation was confirmed by MRI assessment. Both groups (MRI pos and MRI neg) were well balanced in age, sex, BMI and CRP. In the MRI pos group, patients had more severe symptoms of Pso/musculoskeletal complains indicated by increased rates for use of topical or systemic treatments (e.g. MTX 16,7 % vs. 5,7% for Pso, Pso plaques at hands 35,7 vs 15,7%) and NSAID (NSAID 40,5% vs 18,8%) and showed an increased incidence for concomitant diseases (71,4% vs 45,7%). Compared to the PsA (n=143) and Pso (n=95) only group, the MRI pos group showed high similarities in age of onset of Pso (mean age 31,4 vs 31,5 years), in TJC (mean of 6,7 vs 6,2), NSAID use (40,5% vs 32,9%) and BSA (mean 8,9 vs 9,5%) to the diagnosed PsA group and in difference to the Pso only and MRI neg group (table 1).
Conclusion: Early detection of development of musculoskeletal symptoms in PsO patients seem to be associated to the severity of skin symptoms and its need for therapeutic intervention. The FOI and MRI pos group had high similarities in several domains with clinically evident active PsA but not to the Pso only group. Moreover, it seems that the use of systemic treatment with e.g. MTX for Pso has no preventive effect on the development of arthritis.
To cite this abstract in AMA style:
Koehm M, Ohrndorf S, Rossmanith T, Langer H, Backhaus M, Burmester G, Wassenberg S, Köhler B, Burkhardt H, Behrens F. Characteristics of Psoriasis Patients with Subclinical Signs of Musculoskeletal Involvement Detected by Fluorescence Optical Imaging and Confirmed by MRI-assessment [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/characteristics-of-psoriasis-patients-with-subclinical-signs-of-musculoskeletal-involvement-detected-by-fluorescence-optical-imaging-and-confirmed-by-mri-assessment/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/characteristics-of-psoriasis-patients-with-subclinical-signs-of-musculoskeletal-involvement-detected-by-fluorescence-optical-imaging-and-confirmed-by-mri-assessment/