Session Information
Date: Sunday, October 26, 2025
Title: (0731–0764) Vasculitis – Non-ANCA-Associated & Related Disorders Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: GCA is a vasculitis of large and medium-sized arteries that has been well-studied in populations of European descent; however, data on African American (AA) patients remain sparse. We aimed to assess racial differences in demographics, comorbidities, treatment, inflammatory markers, and outcomes in GCA.
Methods: We conducted a retrospective cohort study using TriNetX, a network of de-identified electronic medical records from 102 healthcare organizations. Adults with GCA (ICD-10-CM: M31.5, M31.6) from 2004–2024 were grouped as AA or non-African American (non-AA) (including White, Asian, Hispanic, and others). After 1:1 propensity score matching (33 covariates), cohorts were compared for comorbidities, treatments, inflammatory markers (CRP,ESR at 0/6/12 months), and mortality. Kaplan-Meier survival analysis and Cox regression were used for survival analysis.
Results: 6,507 AA and 40,683 non-AA patients were identified; after matching, 6,505 remained in each group. AA patients were younger at diagnosis (65.1 vs 68.9 years, p< 0.001) and more likely to be female (79 vs.67%, p < 0.001). Hypertension (HTN) and diabetes (DM) were more prevalent in AA, while PMR, anterior ischemic optic neuropathy (AION), and aortic aneurysms were more common in non-AA individuals. Prednisone, MTX, and tocilizumab were comparable between groups (Table 1).After matching and at baseline, CRP was lower in AA than non-AA patients (25.4 vs. 32.7 mg/L, p< 0.001), while ESR was higher (54.5 vs. 42.6 mm/h, p< 0.001). Notably, AA patients continued to exhibit higher ESR and CRP levels at 6 and 12 months (Table 2).Survival analysis revealed a statistically significant difference in mortality between the two groups (Figure 1). Mortality risk was 11.9% in AA vs. 14.3% in non-AA, a difference of –2.4% (p < 0.001). The risk ratio was 0.833 and the odds ratio was 0.811, suggesting a 17–19% relative risk reduction. Kaplan-Meier analysis showed higher survival probability in AA patients (50.44% vs. 36.05%; p = 0.001). Cox regression showed a 14.4% lower mortality hazard (hazard ratio 0.856), with the proportional hazards assumption met.
Conclusion: In our study, AA patients with GCA were younger and more often female at diagnosis compared to non-AA patients. Comorbid HTN and DM were more common in the AA group, while PMR, AION, and aortic aneurysms were more prevalent in the non-AA group. Despite higher inflammatory markers, AA patients had lower mortality and improved survival than other races in this matched cohort. Variations in disease phenotype, comorbidity burden, healthcare access, or other clinical and sociodemographic factors may drive these differences. Further investigation is warranted to explore potential contributors to these outcome differences.
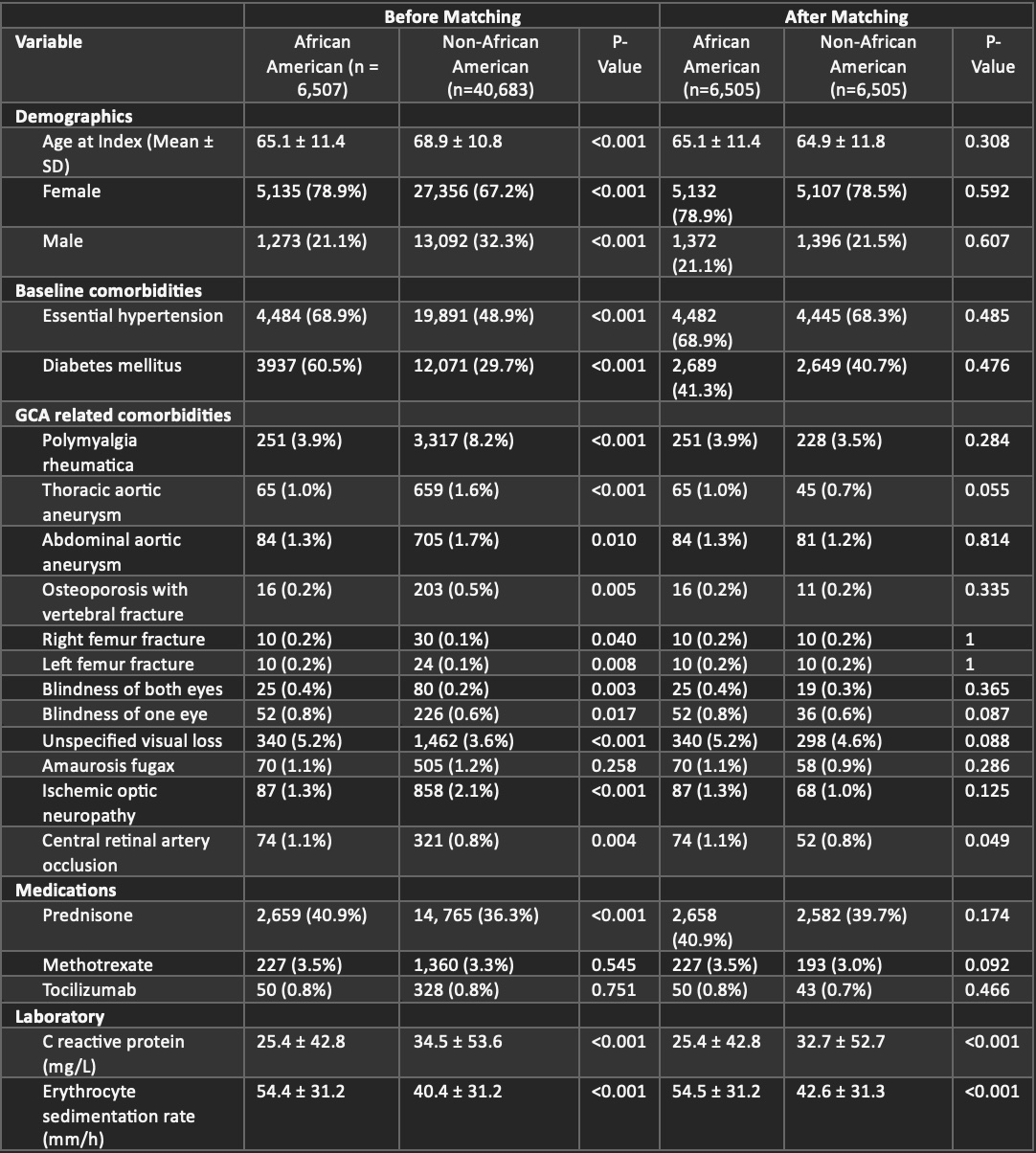 Table 1. Characteristics of African American cohort versus non-African American cohort
Table 1. Characteristics of African American cohort versus non-African American cohort
.jpg) Table 2. Inflammatory marker analysis at time of diagnosis, 6 months, 12 months in African American cohort versus non-African American cohort after matching
Table 2. Inflammatory marker analysis at time of diagnosis, 6 months, 12 months in African American cohort versus non-African American cohort after matching
.jpg) Figure 1. Kaplan-Meier Survival Analysis of Mortality in African American versus non-African American Patient’s with GCA. Key: Purple = African American cohort. Green = non-African American cohort
Figure 1. Kaplan-Meier Survival Analysis of Mortality in African American versus non-African American Patient’s with GCA. Key: Purple = African American cohort. Green = non-African American cohort
To cite this abstract in AMA style:
Nachawati D, Heydari-Kamjani M, Pfeil K, Harper E, Gump M, Frumker L, Daoud A, Pamuk O. Characteristics of African American vs. Non-African American Patients with Giant Cell Arteritis: A Retrospective Cohort Study [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/characteristics-of-african-american-vs-non-african-american-patients-with-giant-cell-arteritis-a-retrospective-cohort-study/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/characteristics-of-african-american-vs-non-african-american-patients-with-giant-cell-arteritis-a-retrospective-cohort-study/
