Session Information
Date: Wednesday, October 24, 2018
Title: 6W018 ACR Abstract: Epidemiology & Pub Health IV: Determinants & Consequences of Tx (2952–2957)
Session Type: ACR Concurrent Abstract Session
Session Time: 11:00AM-12:30PM
The opioid epidemic in the U.S. has led to similar concerns about prescribed opioids in the U.K. In new users, the rate of escalation to more potent opioids is likely to contribute to long-term prescriptions, which in turn may be associated with opioid dependency, addiction and overdose. The scale of such escalation however is unclear in the U.K. We sought to: (i) describe trends of prescribed opioids for non-cancer pain in the UK primary care setting over a 10-year period (ii) assess the sequential transition of opioid strength from index date over a 2-year period. Methods:
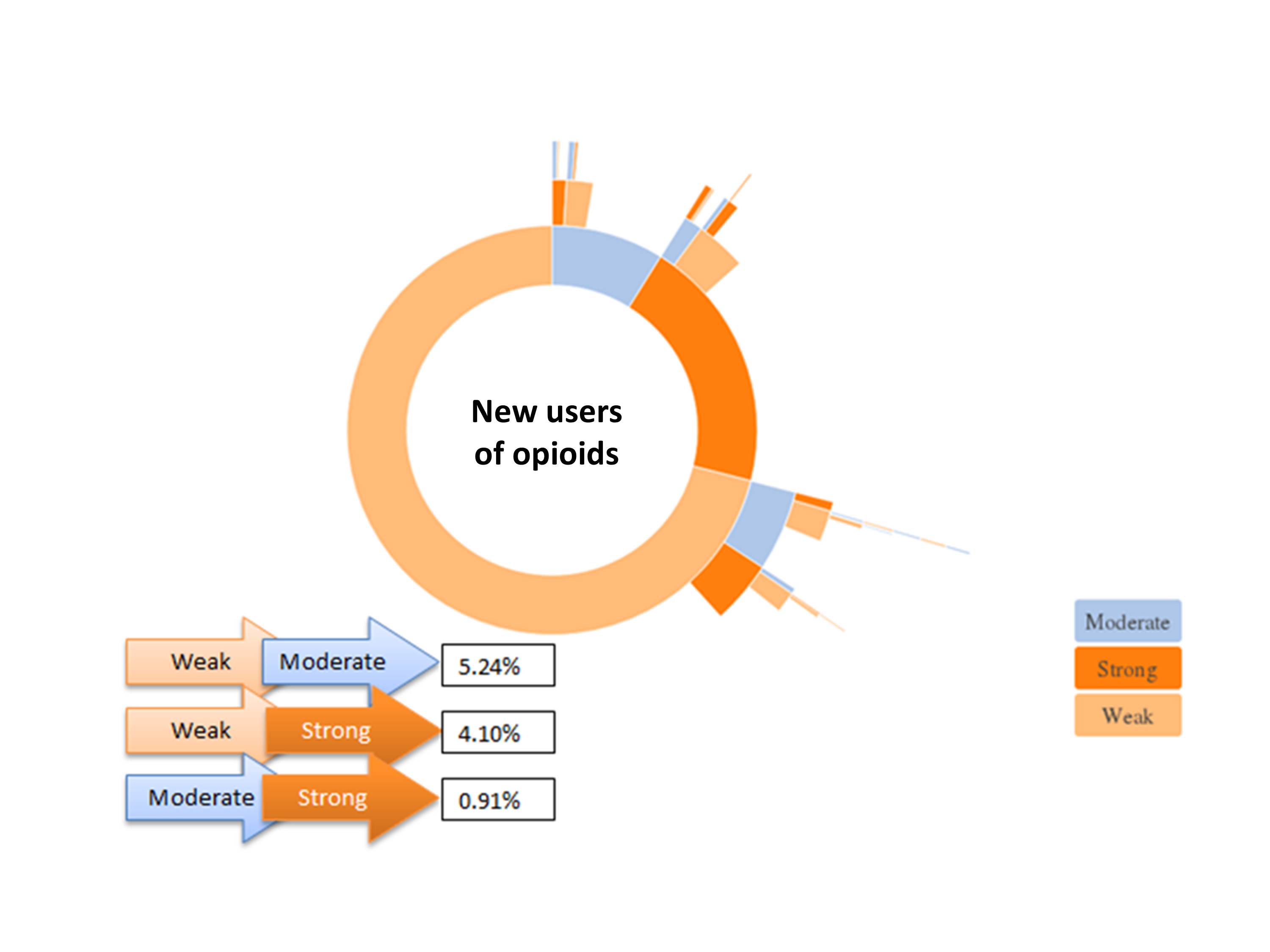
We conducted a retrospective observational study from 1/1/2006 to 31/12/2015 using Clinical Practice Research Datalink (CPRD). New users of opioids, >18 years without cancer in the 2 years prior to index date were identified. The number of prescriptions for each drug were calculated by each calendar year accounting for the number of eligible patients registered in CPRD for that year. Sunburst plots were created to evaluate the sequential transition of opioids over time. A 4-state hidden Markov model was used to estimate the transition probability for individuals escalating to more potent opioids over a 2 year period. States were defined as (i) no drug (ii) weak opioid (codeine, dihydrocodeine) (iii) moderate opioid (tramadol) (iii) strong opioid (all others). Results:
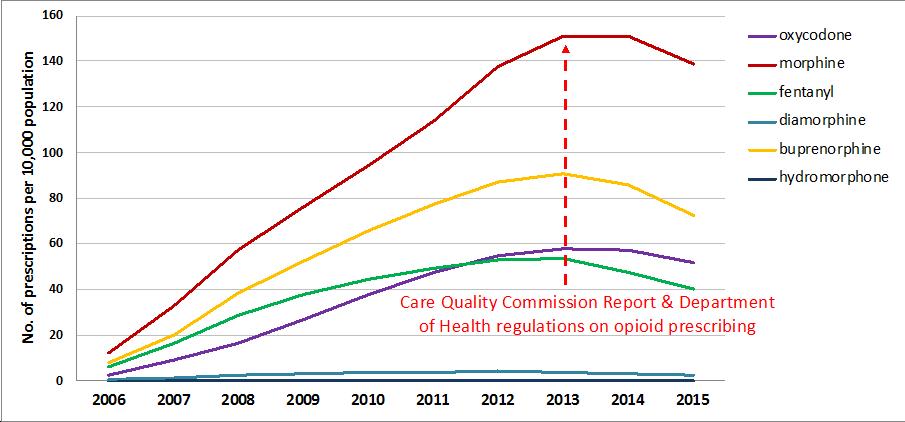
968,797 opioid users were included: mean age (SD) was 55(18) years; 59% being female. New users of opioids were most commonly prescribed codeine (n=685,823; 71.0%), followed by dihydrocodeine (n=166,906; 17.2%), tramadol (n=85,840, 8.8%) with 194,373 (20.1%) strong opioid prescriptions. The rate of prescribing strong opioids/10,000 population increased 12 fold from 2006-2013 (Figure 1). Transitions between opioid strength are demonstrated in Figure 2. Of new users prescribed weak opioids as their first prescription, 5.2% transitioned to moderate opioids, 4.1% to strong opioids over 2 years. Transition probability of moving from weak to strong opioid at a given time point over 2 years was 0.001, whilst staying on a strong opioid (if first prescription) was 0.97.
Conclusion:
Strong opioid prescribing increased till 2013-14 gradually decreasing following UK initiatives to improve monitoring and use of controlled drugs. Although less potent codeine prescriptions made up the majority of first prescriptions, the transition probability of staying on a strong opioid at 2 years remained high if prescribed first as a new user.
Figure 1: Trends in strong opioid utilisation in CPRD by individual opioids
Figure 2: Opioid pathway over 2-year period from index date (excluding repeated prescriptions)
To cite this abstract in AMA style:
Jani M, Birlie Yimer B, Sheppard T, Lunt M, Dixon WG. Changing Trends and Prescribing Patterns in Opioid-Treated Primary Care Patients with Non-Cancer Pain over a 10-Year Period [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/changing-trends-and-prescribing-patterns-in-opioid-treated-primary-care-patients-with-non-cancer-pain-over-a-10-year-period/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/changing-trends-and-prescribing-patterns-in-opioid-treated-primary-care-patients-with-non-cancer-pain-over-a-10-year-period/