Session Information
Session Type: ACR Concurrent Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose:
Semi-quantitative
scoring of magnetic resonance images (MRIs) is a valuable method for performing
multi-feature assessment of the knee joint. The goal of this study was to
investigate the ability of change in semi-quantitative knee MRI biomarkers over
24 months to predict knee osteoarthritis (OA) progression over 48 months.
Methods: Conclusion: Both loss of
This
analysis was done as a part of the fNIH-funded OA Biomarkers Consortium
case-control study. We selected a predetermined number of index knees, one knee
per subject, in four different knee outcome groups: 1) knees with both radiographic
and pain progression; 2) knees with radiographic but not pain progression; 3)
knees with pain but not radiographic progression; 4) knees with neither
radiographic nor pain progression. For the purposes
of this analysis we used the single comparison, comparing knees with both
radiographic and pain progression (cases) vs. everybody else (controls). MRIs
were read according to the MRI Osteoarthritis Knee Score (MOAKS) scoring system
in sequential order unblinded to time point of acquisition but blinded to group
assignment. This analysis focused on change in several joint features: 1) bone
marrow lesions (BMLs), 2) cartilage thickness, 3) cartilage surface area, 4)
effusion-synovitis, 5) meniscus morphology, 6) meniscus extrusion, 7)
osteophytes size, and 8) Hoffa-synovitis. We used logistic regression to
examine the association between each biomarker and case status. Multivariable
models were built in a hierarchical fashion, with the best performing
biomarkers from univariate analyses added to the model first (performance based
on p-value, OR and c-statistics).
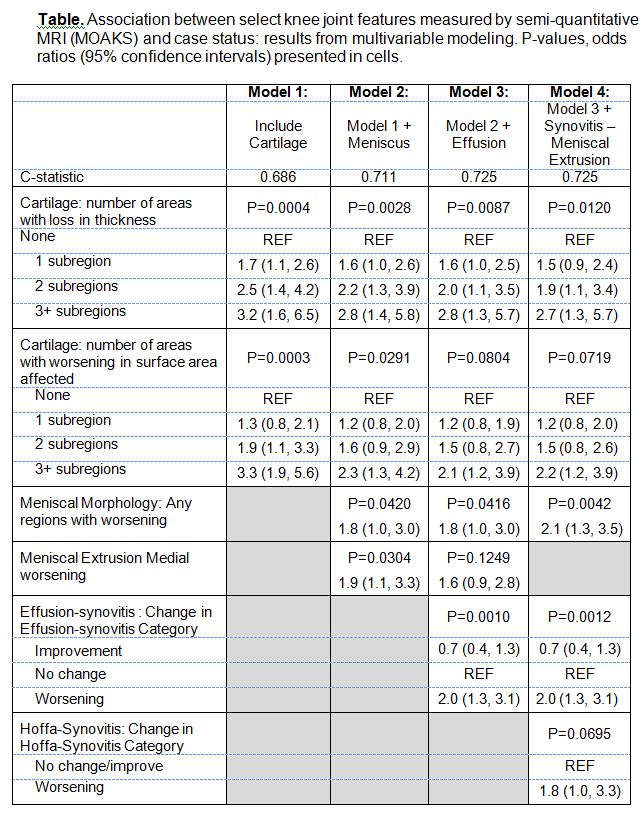
We used
the data from 194 cases and 406 controls, mean age 62 years, 59% females, 51%
K-L 2 and 37% K-L 3. All joint features considered were significantly
associated with case status in univariate analyses, and all features were
progressed to multivariable modeling. We built several hierarchical models with
c-statistics ranging from 0.686 to 0.725 (Table). Results of multivariable
modeling revealed that changes from baseline to 24 months in cartilage
thickness, cartilage surface area, meniscal morphology, effusion-synovitis, and Hoffa-synovitis
independently predicted knee OA progression (case status). BMLs, osteophytes,
and meniscal extrusion did not exhibit a statistically significant association
with being a case in multivariable models when cartilage thickness and surface
area and meniscal morphology were included in the model.
cartilage thickness and cartilage surface area worsening over 24 months were
independently associated with knee OA progression over 48 months. In addition,
changes over 24 months in semi-quantitative measures on MRI related to meniscus
morphology, effusion-synovitis, and Hoffa-synovitis were associated with
progression of knee OA in multivariable models.
To cite this abstract in AMA style:
Collins JE, Losina E, Nevitt MC, Roemer FW, Guermazi A, Lynch JA, Katz JN, Kwoh CK, Jordan JM, Kraus V, Hunter D. Change in Semi-Quantitative Imaging Biomarkers Predicts Knee Osteoarthritis Progression: Data from the Fnih OA Biomarkers Consortium [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/change-in-semi-quantitative-imaging-biomarkers-predicts-knee-osteoarthritis-progression-data-from-the-fnih-oa-biomarkers-consortium/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/change-in-semi-quantitative-imaging-biomarkers-predicts-knee-osteoarthritis-progression-data-from-the-fnih-oa-biomarkers-consortium/