Session Information
Session Type: Abstract Submissions
Session Time: 5:30PM-7:00PM
Background/Purpose: Celiac disease (CD) is a systemic autoimmune disease triggered by gluten. A higher incidence of CD in rheumatology conditions is reported. Joint pain and arthritis are also manifestations of celiac disease. Therefore, the aim of this study is to characterize the presentation of Celiac disease in children with juvenile idiopathic arthritis (JIA).
Methods: Celiac screening for children with JIA has become routine practice in our clinic over the last several years. Patients with JIA and celiac disease who initially presented to the rheumatology clinic were identified via an existing research database and clinic charts. Charts were reviewed to characterize the presentation of joint and celiac disease.
Results: A total of 10 children with JIA had confirmed celiac disease. All 10 had a positive anti-tissue transglutaminase antibody with 9 having greater than detectable levels. In 9 patients the diagnosis was confirmed via biopsy and 1* via genetic testing. Median age at JIA diagnosis was 8 years (3-16). The time interval between JIA diagnosis and subsequent celiac diagnosis ranged from 0-12 years (median 0.5). Median number of joints involved at celiac diagnosis was 2.5 (1-40), with greater than half being polyarticular pattern. 9 patients had no gastrointestinal complaints and were detected on routine screening (although after celiac diagnosis 4 retrospectively reported mild abdominal pain which was not severe enough to seek medical care). 1 patient+was tested due to chronic abdominal pain and family history. None had a classic presentation of celiac disease with diarrhea and poor weight gain. 6 of 10 patients were ANA positive. 1 of 10 was RF positive. 8 of 10 patients were tested for HLA-B27, 1 was positive. 4 patients were treated with disease-modifying anti-rheumatic drugs (DMARDs), while the remainder were treated with steroid joint injections and NSAIDs. 6 of 10 patients had joint symptoms improvement with initiation of a gluten free diet. Of these, only 1 was treated with DMARDs.
Conclusion: The presentation of celiac disease in children with JIA is varied. It can present at any age and with any number of joints. Importantly, there may be minimal or no gastrointestinal symptoms. Furthermore, our results suggest that for children with celiac disease and arthritis, initiation of a gluten-free diet may result in improved joint control. As untreated celiac disease can lead to significant morbidity, and treatment of celiac disease may improve joint disease, we recommend providers consider celiac screening in any child presenting with JIA.
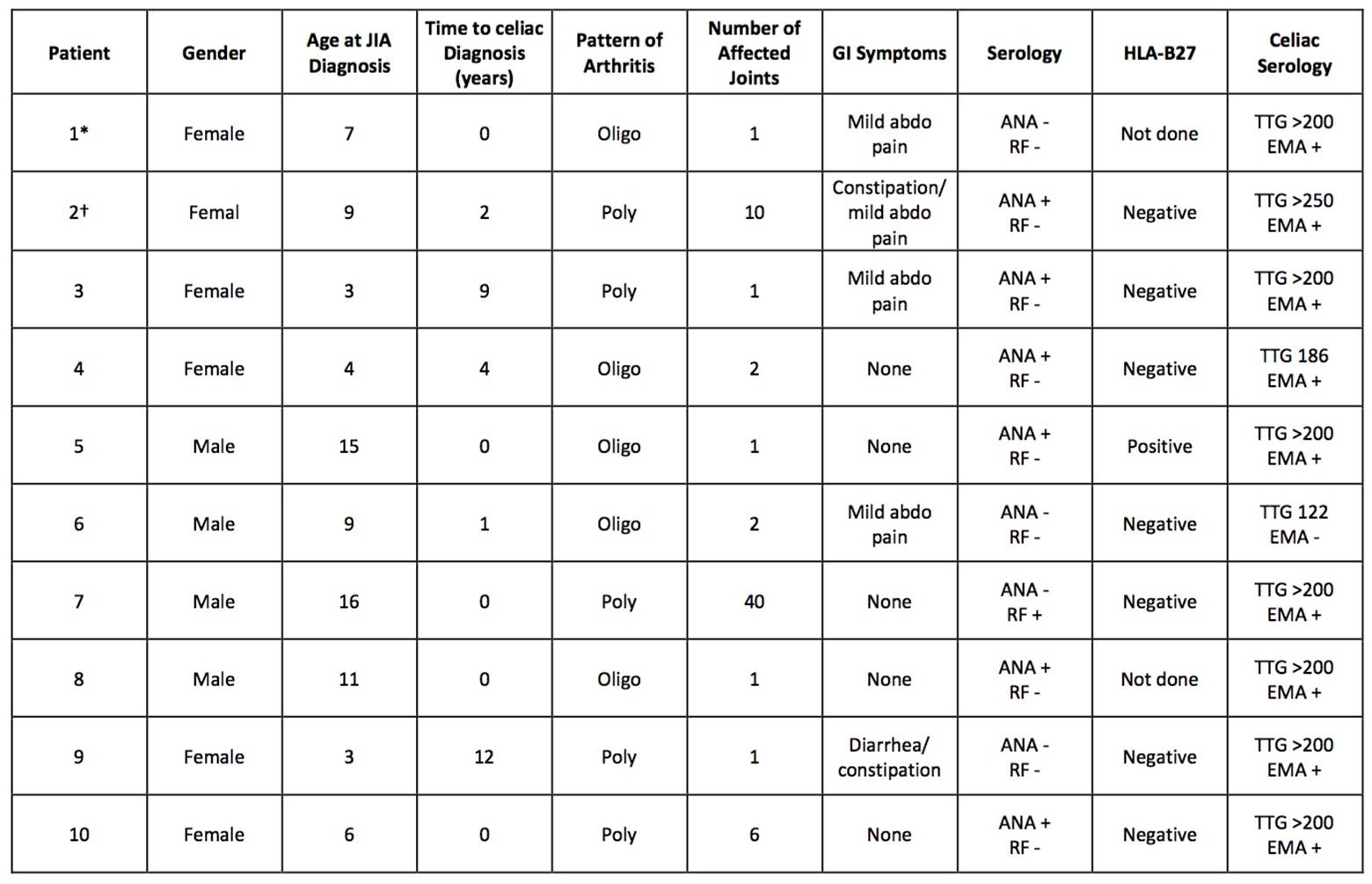 Table 1. Clinical presentation of children with juvenile idiopathic arthritis and celiac disease.
Table 1. Clinical presentation of children with juvenile idiopathic arthritis and celiac disease.
To cite this abstract in AMA style:
Smith A, Johnson N, Luca N, Veeramreddy D, Schmeling H. Celiac Disease in Children Diagnosed with Juvenile Idiopathic Arthritis [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 4). https://acrabstracts.org/abstract/celiac-disease-in-children-diagnosed-with-juvenile-idiopathic-arthritis/. Accessed .« Back to 2017 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/celiac-disease-in-children-diagnosed-with-juvenile-idiopathic-arthritis/
