Session Information
Date: Monday, November 11, 2019
Title: Epidemiology & Public Health Poster II: Spondyloarthritis & Connective Tissue Disease
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Survival has improved in ANCA-associated vasculitis (AAV) with evolving management strategies, but patients remain at an increased risk of death compared to the general population. Contemporary data regarding cause of death in AAV remain scarce and although growing appreciation of differences between patients with different ANCA types exists, no analysis has evaluated causes of death among patients with ANCA directed against myeloperoxidase (i.e., MPO-ANCA) as opposed to proteinase-3 (PR3-ANCA). We evaluated overall causes of death in a contemporary inception cohort of AAV patients, stratifying the analysis according to ANCA type.
Methods: We identified a consecutive inception cohort of patients newly-diagnosed with AAV evaluated between 2002 and 2017 in the Partners HealthCare System in Boston and determined vital status through the National Death Index. Cause of death was extracted from death certificates and organized using a validated schema that clusters diagnoses into clinically meaningful categories, such as cardiovascular disease (CVD), infection, malignancy, renal disease, and non-infectious respiratory disease based on ICD-9 or ICD-10 codes. We determined cumulative incidence of overall and cause-specific mortality and standardized mortality ratios (SMR) compared to the general population. We compared MPO-ANCA+ and PR3-ANCA+ cases using Cox regression models.
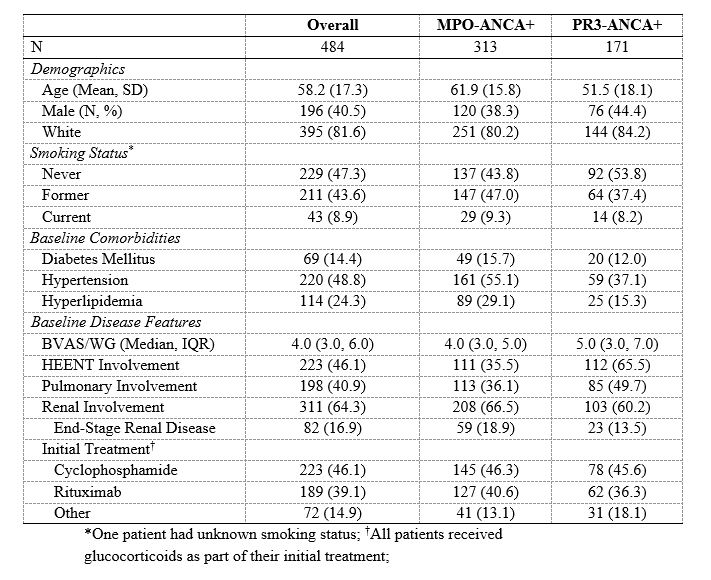
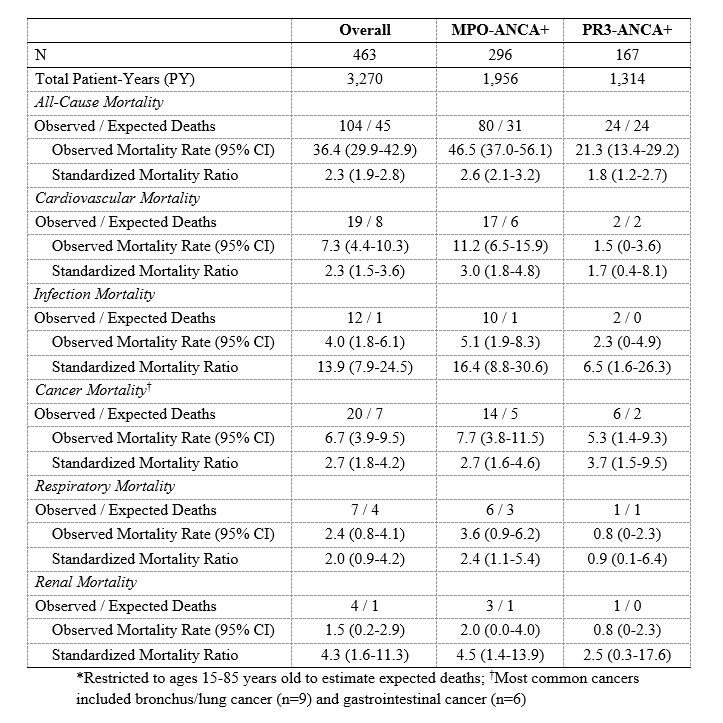
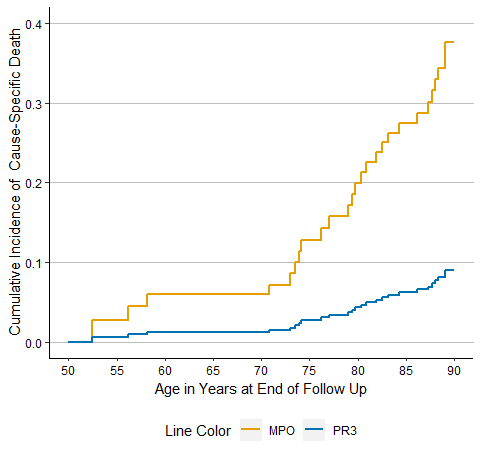
Results: The study population consisted of 484 patients with a mean age of 58 years at diagnosis (Table 1). 40% were male, 65% were MPO-ANCA+, and 65% had renal involvement. The median baseline BVAS/WG was 4.0. During 3,385 person-years (PY) of follow-up, 130 patients died, yielding a mortality rate of 38.4/1,000 PY and a SMR of 2.3 (95% CI: 1.9-2.8). The most common cause of death was CVD (10-year cumulative incidence 7.1%), followed by malignancy (5.9%) and infection (4.1%). Of the common causes of death, the SMR for death due to infection was greatest for both MPO- and PR3-ANCA cases (16.4 [95% CI: 8.8-30.6] and 6.5 [95% CI: 1.6-26.3], respectively). MPO-ANCA patients had a significantly elevated SMR for death due to CVD (3.0 [95% CI: 1.8-4.8]), respiratory disease (2.4 [95% CI: 1.1-5.4]), and renal disease (4.5 [95% CI: 1.4-13.9]); however, these causes were not significant among PR3-ANCA+ patients (Table 2). In contrast, PR3-ANCA+ subjects had a greater SMR for malignancy-associated mortality than MPO-ANCA+ subjects (3.7 [95% CI: 1.5-9.5] vs 2.7 [95% CI: 1.6-4.6]). MPO- and PR3-ANCA cases had similar risk of all-cause mortality (aHR 1.3 [95% CI: 0.8-1.9], p=0.2). However, MPO-ANCA+ cases had a higher risk of CV death (HR 4.52 [95% CI: 1.00-20.33], p=0.049) compared to those who were PR3-ANCA+ (Figure 1).
Conclusion: The premature mortality risk in AAV is explained by CVD, infection, malignancy, and renal death. CVD is the most common cause of death but the largest excess mortality risk in AAV is associated with infection. MPO-ANCA+ subjects are at higher risk of CVD death than PR3-ANCA+ subjects. Our findings highlight the importance of CVD as a cause of death, especially for MPO-ANCA+ subjects, but also emphasize the importance of infections, malignancies, renal failure, and respiratory issues to excess mortality in AAV.
To cite this abstract in AMA style:
Wallace Z, Fu X, Harkness T, Stone J, Zhang Y, Choi H. Causes of Death in ANCA-Associated Vasculitis According to ANCA Type [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/causes-of-death-in-anca-associated-vasculitis-according-to-anca-type/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/causes-of-death-in-anca-associated-vasculitis-according-to-anca-type/