Session Information
Date: Tuesday, November 7, 2017
Title: Epidemiology and Public Health Poster III: Rheumatic Disease Risk and Outcomes
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: The major SARD have an increased mortality compared to the general population. It is well known that the main causes of death in Systemic Lupus Erythematosus (SLE) are infections (INF), cardiovascular events (CV), neoplasia (NEO) and disease activity. However, the compared mortality of Mixed Connective Tissue Disease (MCTD), Systemic Sclerosis (SSc), Poly/Dermatomyositis (PM/DM), overlap syndromes (OS), Sjögren’s syndrome (SS), Antiphospholipid syndrome (APS), systemic vasculitis (SV), and undifferentiated or incomplete Connective Tissue Disease (UCTD) is poorly described. To analyze the causes of death and the autoantibodies (AAB) profile among the SARD.
Methods: This was a single center, prospective and observational study. Mortality by all causes and relationship with AAB profile were analyzed in patients diagnosed of SLE, MCTD, SSc, PM/DM, OS (simultaneous or sequential criteria of 2 or more SARD), SS, APS, SV and UCTD or incomplete SARD (at least one clinical criterion of the classification criteria and a related antibody of any of the SARD). Data were obtained from the “Systemic Autoimmune Rheumatic Diseases Registry” of a tertiary referral hospital from 1986 to 2016. Patients with rheumatoid arthritis were excluded. The SARD registry counts with the institutional review board approval.
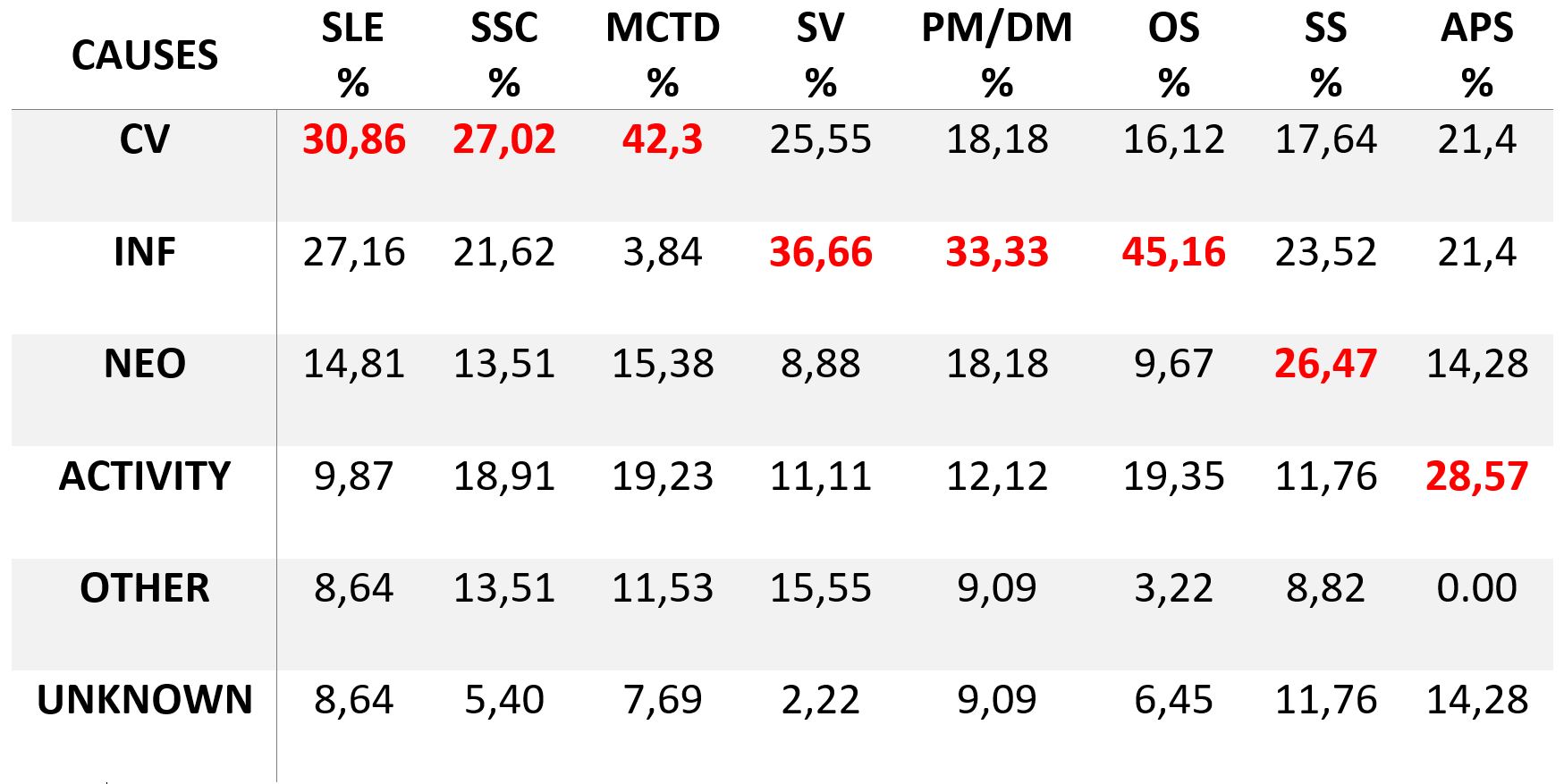
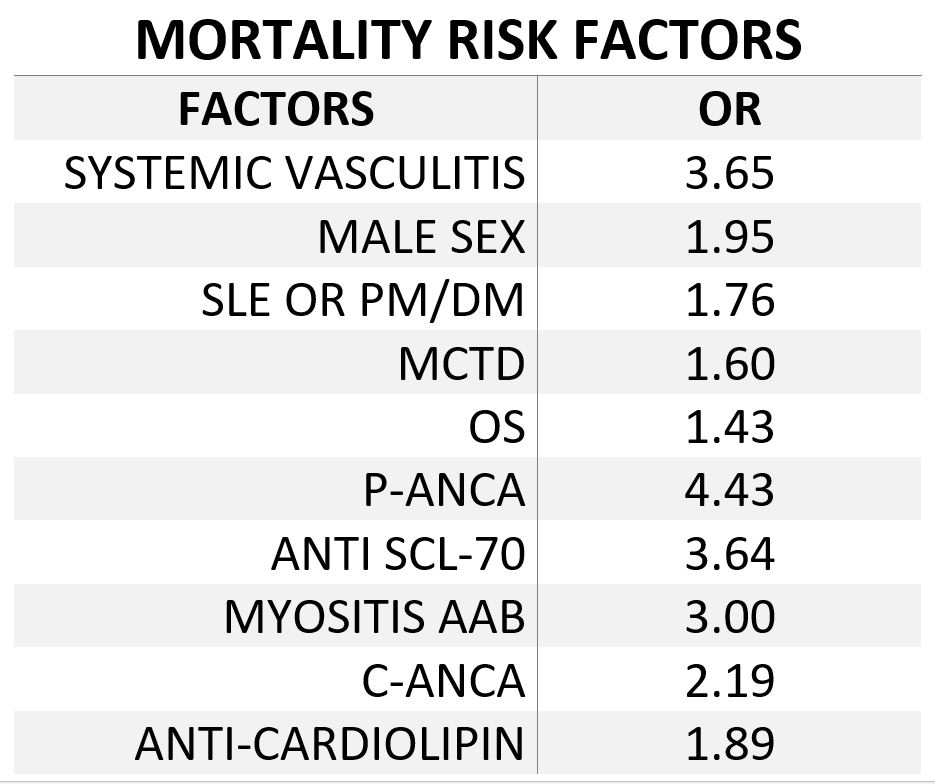
Results: 1750 patients were included, of whom 1453 (83%) were women. Five hundred fifty six SLE, 125 SSc, 111 PM/DM, 91 OS, 90 MCTD, 250 SS, 71 APS, 211 SV, 117 UCTD and 128 losses to follow-up, the global follow up rate was 92.7%. A global mortality of 350 (20%) cases was observed: 101 INF (28,8%), 89 CV (25,4%), 51 NEO (14,5%), 45 due to disease activity (12,8%), 41 other causes (11,7%) and 23 from unknown causes (6,5%). Table 1 shows detailed mortality causes compared by diseases. A higher mortality was associated (p<0,05) with older patients (71 years, 20-96), SV (OR 3,65), male patients (OR 1,95), SSC/PM/DM (OR 1,76), MCTD (OR 1,6) and OS (OR 1,43). AAB to pANCA (OR 4,43), anti‐topoisomerase I (OR 3,64), myositis-specific AAB (OR 3.0), cANCA (OR 2,19) and anticardiolipin (OR 1,89) were associated with poorer survival. A higher survival rate was observed in patients with SLE (OR 1,7), SS (OR 1,69) and UCTD (OR 15,57) (p<0,05).
Conclusion: The main causes of death among SARD patients are CV (MCTD, SLE, and SSC), severe infections (OS, SV, and PM/DM), disease activity (APS) and neoplasia (SS). A higher mortality is observed among ANCA positive SV, anti‐topoisomerase I positive SSC, MCTD, OS, anticardiolipin and myositis-specific positive patients.
To cite this abstract in AMA style:
Ovalles-Bonilla JG, Fernández-Berrizbeitia O, Martínez-Barrio J, Valor L, Hernández D, Janta I, Serrano B, Saez C, Gonzalez R, Correyero M, García L, López-Cerón A, Silva A, Nieto JC, González C, Monteagudo I, López Longo FJ. Causes of Death in 350 Patients with Systemic Autoimmune Rheumatic Diseases [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/causes-of-death-in-350-patients-with-systemic-autoimmune-rheumatic-diseases/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/causes-of-death-in-350-patients-with-systemic-autoimmune-rheumatic-diseases/