Session Information
Session Type: ACR/ARP Abstract Session
Session Time: 11:00AM-12:30PM
Background/Purpose: Legalization of cannabis use is rapidly increasing worldwide, raising the need to evaluate trends and medical implications. A systematic literature review showed inconsistent results on tolerability and safety of cannabis-based medicines for any chronic pain [1]. Additionally, little is known about the use and effectiveness of cannabis in rheumatic diseases [2]. We sought to evaluate the trends of cannabis use and associations with rheumatic disease characteristics in a US-wide registry.
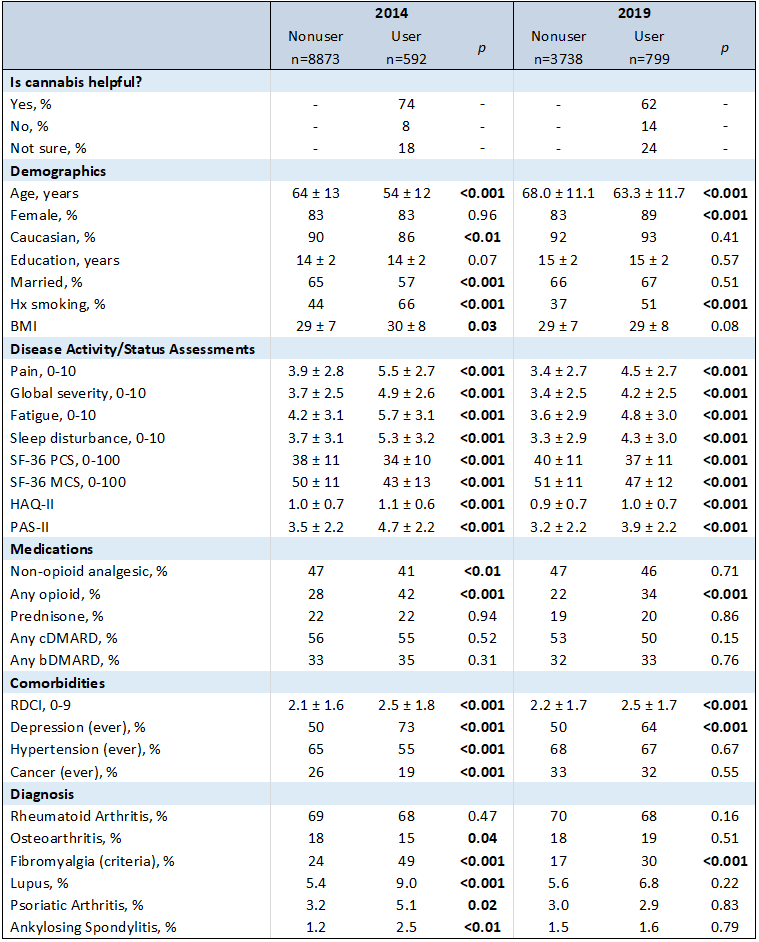
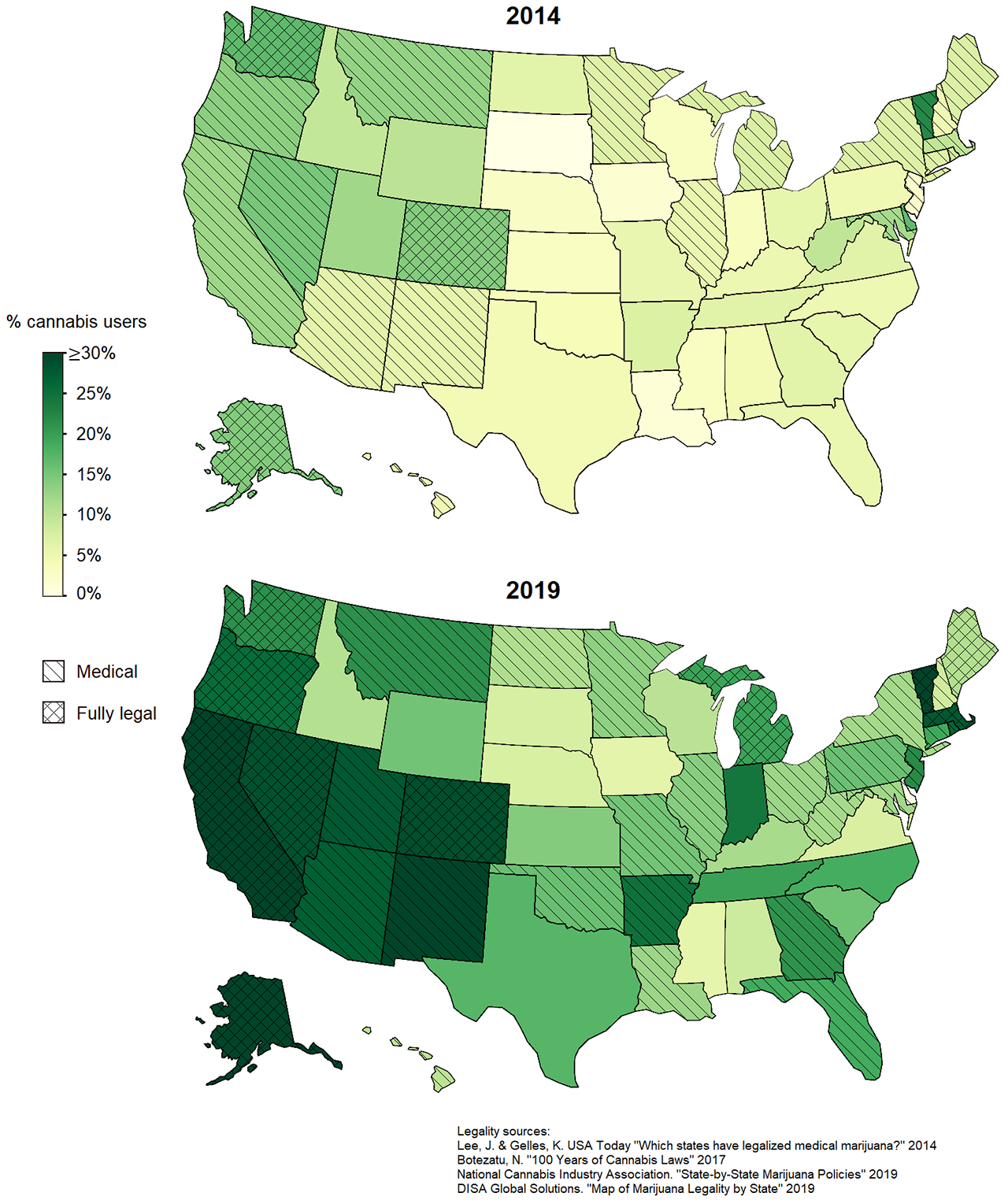
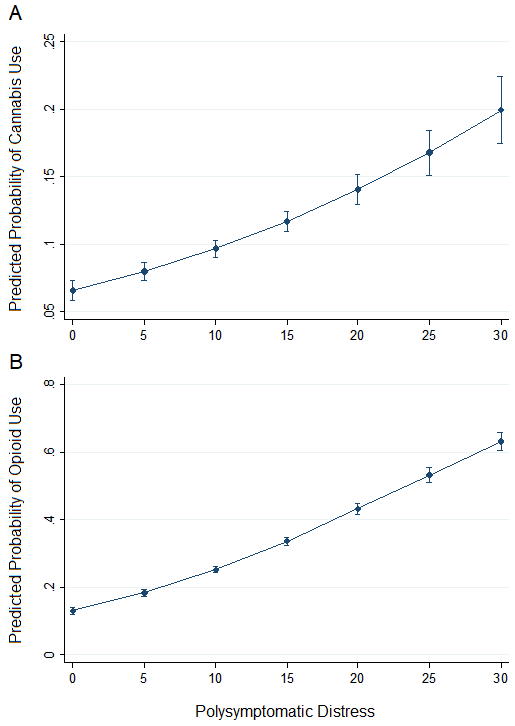
Methods: Study patients were participants in FORWARD, The National Databank for Rheumatic Diseases, a longitudinal study of rheumatic disease outcomes, who indicated in a 2014 and/or 2019 questionnaire whether they had ever used marijuana, cannabis, or cannabidiol (hereafter cannabis) for symptom relief, and if so, whether they found it helpful. Demographics, disease activity/status assessments (PRO), medications, comorbidities, and diagnosis were compared between cannabis users and nonusers in 2014 and 2019. Significance was assessed using t-tests and Chi-square tests as appropriate. Choropleth maps were generated based on prevalence of cannabis use in each US state. Logistic regression models were generated to determine the probability of cannabis or opioid use by polysymptomatic distress (the score used to determine whether fibromyalgia criteria are met).
Results: Among the 11,006 unique respondents, the prevalence of past or current cannabis use has increased from 6.3% in 2014 to 17.6% in 2019. At both time points, patients reporting use were younger, had worse measures on all PROs, and were more likely to have a history of smoking cigarettes, have fibromyalgia, report a history of depression, and report opioid use (Table 1). In 2014, users were also less likely to be Caucasian, married, and have health insurance. In 2019 there were fewer demographic differences. Most patients reported that cannabis was helpful in relieving symptoms (74% in 2014 and 62% in 2019). Since 2014, prevalence of use increased in 49 of 50 US states, with the highest prevalence in and near states where cannabis use is legal (Figure 1). Logistic regression models indicate that the probability of cannabis use increases with increasing polysymptomatic distress, and the same is true for opioid use (Figure 2).
Conclusion: Reported cannabis use among patients with rheumatic diseases has increased significantly, and most patients stated it was helpful for symptom relief. Patients who tried cannabis tended to have worse pain, disease activity, and symptoms and were taking more analgesics. While interpretation of cannabis effectiveness is beyond our study’s scope, the association with prior opioid use and polysymptomatic distress highlights areas for future work.
References:
1 Häuser W W, Petzke F Fitzcharles MA; Efficacy, tolerability and safety of cannabis-based medicines for chronic pain management – An overview of systematic reviews. European j Pain, volume 22, issue 3, 2018.
2 Fitzcharles MA, Niaki Z, Omid O, Hauser WW, Hazlewood G, et.al. A Pragmatic Approach for Medical Cannabis and Patients with Rheumatic Diseases.;2019 Jan 15; J. Rheumatol.
To cite this abstract in AMA style:
Wipfler K, Simon T, Katz P, Wolfe F, Michaud K. Cannabis Use Among Patients in a Large US Rheumatic Disease Registry [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/cannabis-use-among-patients-in-a-large-us-rheumatic-disease-registry/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/cannabis-use-among-patients-in-a-large-us-rheumatic-disease-registry/