Session Information
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Cardiovascular (CV) manifestations of Rheumatological inflammatory diseases have become increasingly recognized, and, in some patients, might even constitute the initial presentation of a Rheumatological disorder. The objective of this study was to examine the CV co-morbidities in Medicare beneficiaries using 2013 aggregated Part B Medicare data.
Methods: Aggregated tables by physician national identifier as well as State and HCPCS codes have been made available with beneficiary demographic and health characteristics. The 2013 data is based on all Medicare part B non-institutional claims. Since claims data is used for payment, it is felt that the documentation of disease processes is reliable. For each chronic condition outlined in table, the prevalence was averaged across all providers. Population numbers were calculated by multiplying unique beneficiary counts by percent prevalence. National disease prevalence percentages and numbers were obtained from the Medicare chronic conditions warehouse. Complete cases of data where then extracted to examine state trends. Beneficiary numbers with the respective disease were calculated, aggregated and plotted by state.
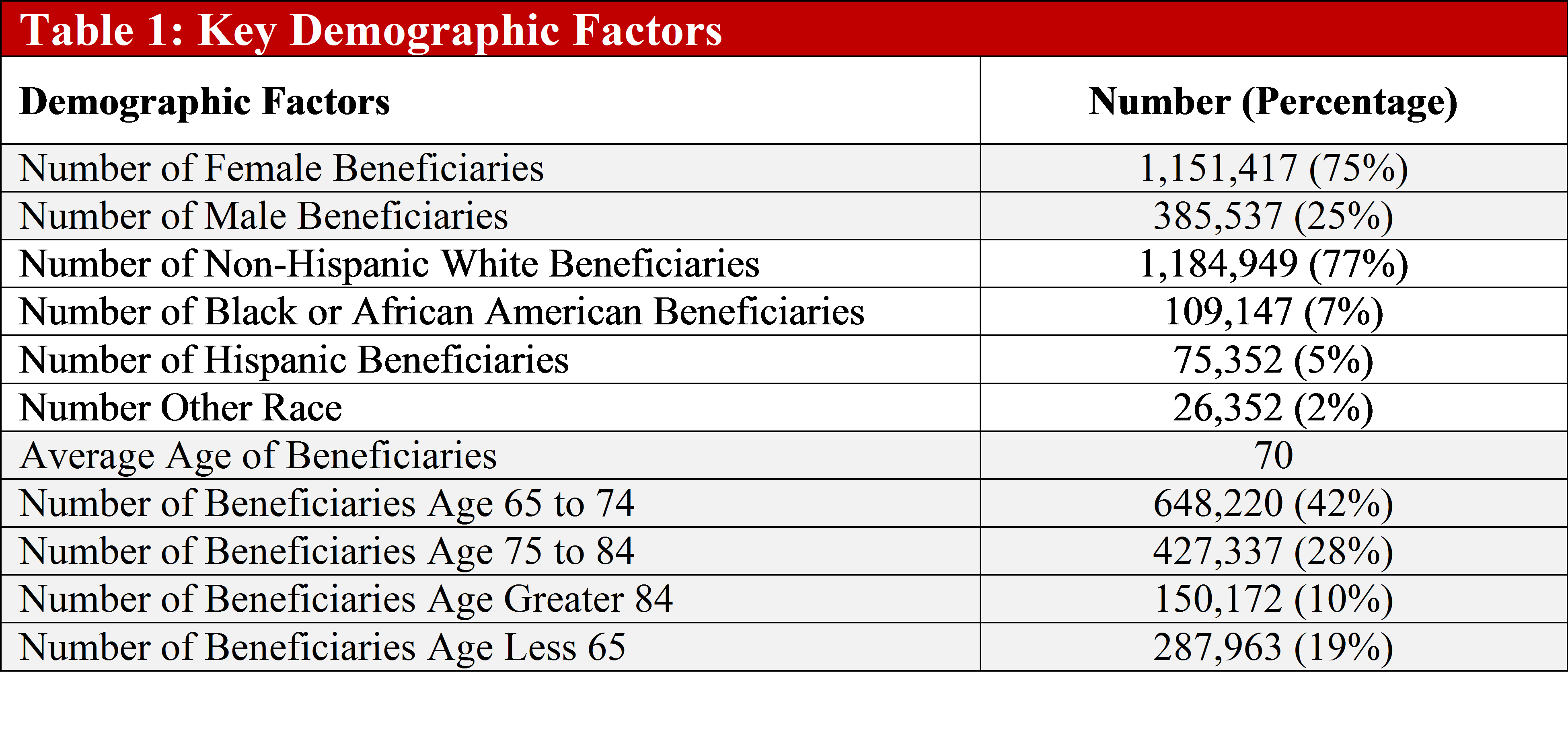
Results: Mean beneficiary age was 70 years with the majority of females, white, and aged between 65 to 74 (Table 1). The prevalence of hypertension (65%) and hyperlipidemias (53%) were highest CV comorbidities and were higher compared to the national figures. (Table 1). Moreover, all comorbidities were higher in the rheumatology beneficiary population compared to the national population. Ischemic heart disease prevalence was 32% compared to 19% in the national population. Of note, the prevalence of diabetes was slightly lower (29%) than the ischemic heart disease in both populations. State trends revealed that the highest prevalence of cardiovascular comorbidities was in Florida, even though California has the largest beneficiary population (Figure 1). The pattern of prevalence of hypertension and hyperlipidemia were closely related over all the states.
Conclusion: The past decade has brought many new insights regarding excessive burden of CV co-morbidities associated with Rheumatological inflammatory diseases. This study has highlighted strong evidence of high CV co-morbidities prevalence among Medicare beneficiaries placing this group under high CV risk category based on the recent national guidelines. Taken together, these findings underscore the complexity of the Rheumatological inflammatory diseases and highlight the key role of further epidemiological research in understanding these intriguing conditions. In addition, priority should be given to pay attention to control of factors affecting CV co-morbidities in this high-risk population.
To cite this abstract in AMA style:
Kaeley GS, Dodani S. Call to Action: Cardiovascular Comorbidities in Medicare Rheumatology Beneficiaries [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/call-to-action-cardiovascular-comorbidities-in-medicare-rheumatology-beneficiaries/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/call-to-action-cardiovascular-comorbidities-in-medicare-rheumatology-beneficiaries/