Session Information
Date: Monday, November 9, 2015
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Rheumatoid arthritis (RA) is a systemic inflammatory disease resulting in significant healthcare resource utilization (HRCU) and cost. Data on elderly RA patients are generally limited. This study aimed to estimate the burden of RA in the US elderly by comparing comorbidities, HCRU, and cost among elderly RA patients with elderly non-RA patients.
Methods: Using Medicare fee-for-service claims data from 2010 through 2013, this was a retrospective study of RA patients aged ≥ 65 years with ≥ 2 medical claims with a diagnosis of RA (ICD-9-CM 714.xx) and ≥ 1 pharmacy claim for a disease-modifying antirheumatic drug (DMARD, biologic and/or conventional synthetic), and a control cohort of non-RA elderly patients, 1:1 matched on age, gender, race, and region. The index date was the date of the first prescription DMARD for RA patients, and randomized assigned for non-RA patients. Prevalence of comorbidities was assessed for a 12-month period prior to the index. All-cause and RA-related (defined based on RA diagnosis and treatment) HCRU and costs during the 12-month post-index period were compared between elderly patients with RA and matched controls.
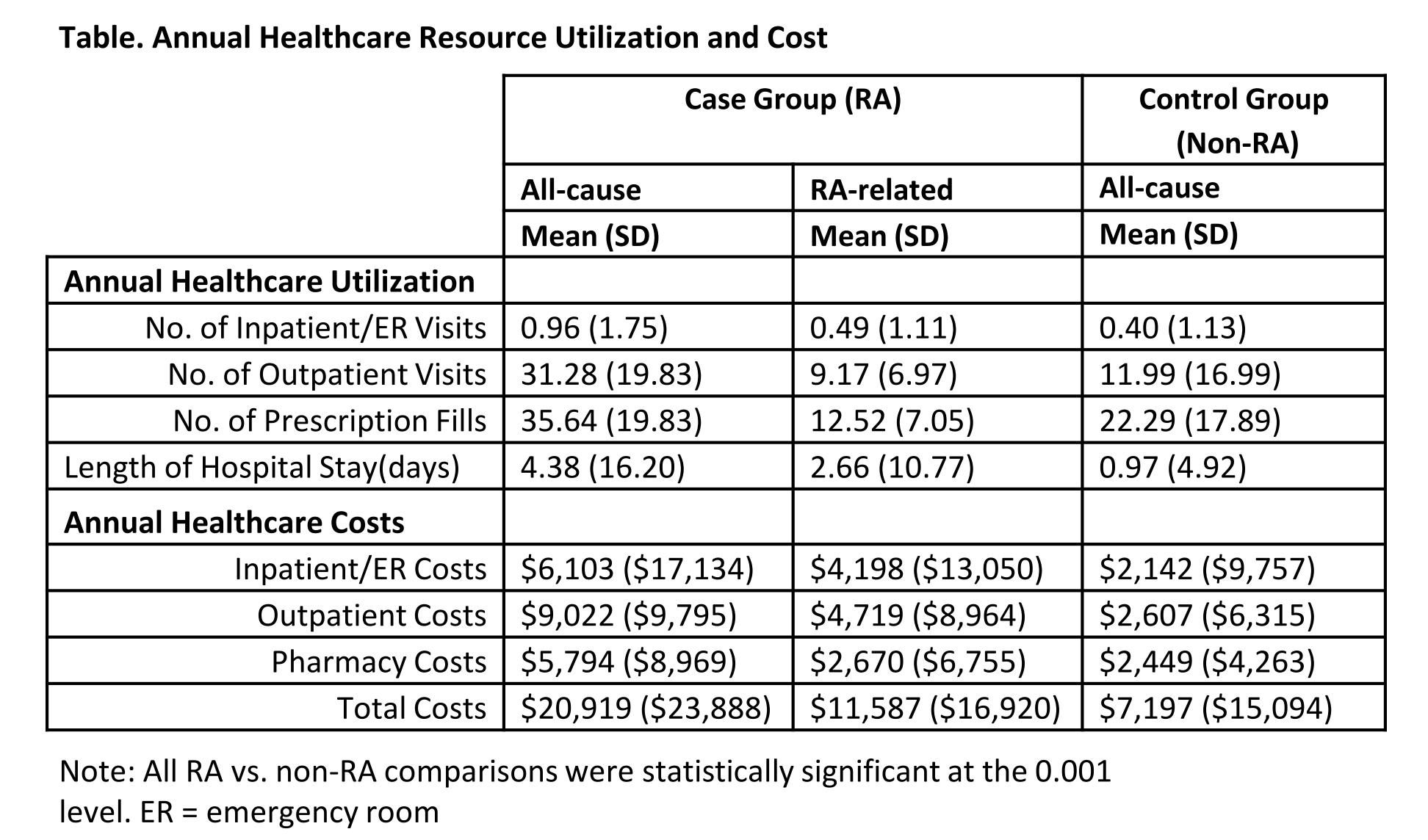
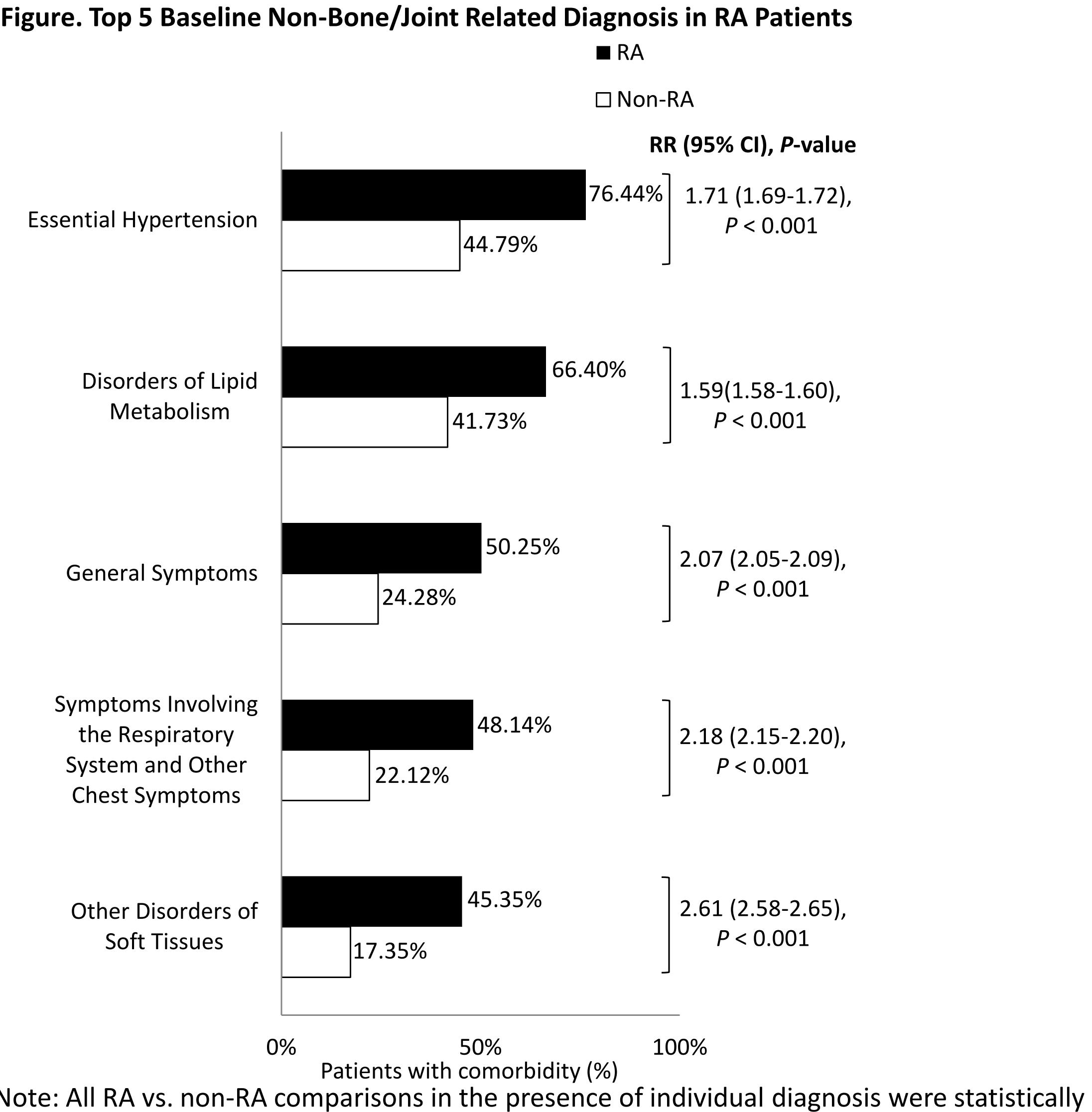
Results: The matched cohorts included a total of 231,734 patients (elderly RA, n = 115,867; control, n = 115,867) with average age 75.2 years, 79.4% women, 86.2% Caucasian, and 41.3% living in the South. Compared with non-RA elderly, RA elderly had significantly greater overall comorbidity burden (Charlson Comorbidity Index excluding RA: 1.86 vs. 1.00, P < 0.0001) and individual baseline comorbidities including hypertension, hyperlipidemia, diabetes, respiratory disease, osteoporosis, and cardiovascular diseases (all P < 0.0001). The top 5 non-bone/joint-related diagnoses among RA patients were essential hypertension, disorders of lipid metabolism, general symptoms, symptoms involving the respiratory system and other chest symptoms, and other disorders of soft tissue (Figure). Elderly RA patients had significantly more HCRU than non-RA patients, resulting in nearly 3-fold higher annual healthcare costs, with half being RA-related (Table). After controlling for differences in patient characteristics and comorbidities, the adjusted total mean annual costs for RA patients were still more than double as that of non-RA patients ($16,374 vs. $6,712, P < 0.0001).
Conclusion: Among US elderly patients, RA was associated with significantly greater burden of comorbidities, HCRU and costs, as compared with elderly patients without RA. RA was a major driver of the overall healthcare use and cost.
To cite this abstract in AMA style:
Chen CI, Wang L, Wei W, Yuce H, Phillips K. Burden of Rheumatoid Arthritis in the US Elderly Population: Comorbidities, Healthcare Resource Utilization, and Cost [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/burden-of-rheumatoid-arthritis-in-the-us-elderly-population-comorbidities-healthcare-resource-utilization-and-cost/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/burden-of-rheumatoid-arthritis-in-the-us-elderly-population-comorbidities-healthcare-resource-utilization-and-cost/