Session Information
Date: Monday, October 27, 2025
Title: (1467–1516) Systemic Lupus Erythematosus – Diagnosis, Manifestations, & Outcomes Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: A recent meta-analysis found an overall 2.87-fold increase in all-cause mortality in systemic lupus erythematosus (SLE) with cause-specific increases in renal disease, infections, cardiovascular disease, stroke and cancer. An increase in mortality due to lupus nephritis was found between 2015-2020. Yen et al examined SLE mortality in the United States from 1968 to 2013. Multiple logistic regression found sex (male), race (blacks) and region (the South) were associated with SLE mortality. We evaluated the role of different demographic variables on mortality outcomes in systemic lupus erythematosus (SLE) in a large single-center cohort.
Methods: Using data from the cohort and the National Death Index, we analyzed demographic and clinical information to discover links between demographic characteristics and mortality. Cox proportional hazards models were used to assess the independent effects of age, gender, race/ethnicity, education and socioeconomic status on mortality risk while controlling for disease activity and comorbidities. Given the strong non-linear relationship between age and mortality, all estimated associations with mortality are adjusted for age at diagnosis and age at diagnosis squared.
Results: Of the 3,021 patients included from the cohort, 628 deaths were recorded. They were 89% female, 34% had a household income of more than $40,000, and 82% had 12 years or more years of education. They were 48% White, 50% Black, 1% East Asian and 1% Other or mixed racial background. Male gender (p=0.0098), Black race vs White (p < 0.0001), less than 12 years of education (p < 0.0001), and household income of less than or equal to $40,000 (p < 0.0001) were associated with increased mortality in both univariate (Table 1) and multivariable (Table 2) models. Decreased mortality was observed for those diagnosed with lupus after 1990 (Table 1, Table 2). White race with high income had the lowest mortality, and black race with low income had the highest mortality (Figure 1).
Conclusion: Patel et al, in a meta-analysis, found that Blacks had higher mortality than Whites, but could not comment on socioeconomic factors. In the Eight Americas study, Falasinnu et al found that Blacks sharing the same social and geographic contexts as Whites had higher mortality, but SLE mortality did not vary between socially advantaged and disadvantaged Blacks. Our results, using individual patient data to measure socioeconomic status in 2 ways (household income and education) clearly contradict the Eight Americas study. Race and socioeconomic status both played a role in mortality risk in SLE, even in a single center of excellence (where access to care and medication were not issues). Our single center study was able to use actual individual patient household income and education, and not infer it from zip codes or county of residence. Black race with high income had better survival than white race with low income.
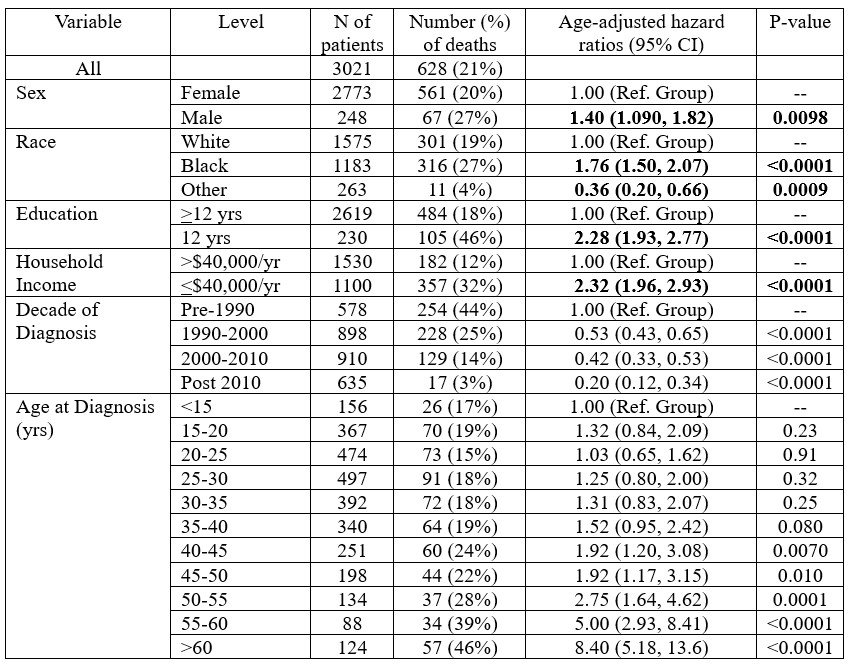 Table 1. Predictors of Mortality based on a Cox Proportional Hazard Model
Table 1. Predictors of Mortality based on a Cox Proportional Hazard Model
.jpg) Table 2. Multivariable Model of Predictors of Mortality
Table 2. Multivariable Model of Predictors of Mortality
.jpg) Figure 1. Estimated probability of survival by years since diagnosis by Race and Income
Figure 1. Estimated probability of survival by years since diagnosis by Race and Income
To cite this abstract in AMA style:
Kaur G, Goldman D, Fava A, Magder L, Petri M. Both Race and Socioeconomic Status Affect Mortality in SLE [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/both-race-and-socioeconomic-status-affect-mortality-in-sle/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/both-race-and-socioeconomic-status-affect-mortality-in-sle/
