Session Information
Date: Saturday, November 6, 2021
Title: Abstracts: Osteoporosis & Metabolic Bone Disease – Basic & Clinical Science (0445–0448)
Session Type: Abstract Session
Session Time: 10:15AM-10:30AM
Background/Purpose: Impaired bone quality and strength estimated by high resolution peripheral quantitative computer tomography (HR-pQCT) in patients with rheumatic diseases on long-term glucocorticoid (LTGC) therapy could discriminate patients with and without fragility fracture, independent of areal bone mineral density (aBMD) (1). The aim of this study was to ascertain whether compromised vBMD, bone microarchitecture and estimated bone strength at baseline in rheumatic disease patients on LTGC therapy could predict incident fragility fracture.
Methods: Two hundred and twenty rheumatological patients on LTGC with (n=110) or without (n=110) fragility fracture who participated in a cross-sectional study with dual-energy X-ray absorptiometry (DXA) and HR-pQCT done between 2014-2016 were invited to have a 5th year follow-up assessment. All patients had a repeat assessment with 1) aBMD and 2) HR-pQCT 3) spine radiographs. The occurrence of new fragility fracture after 5 years was documented. The baseline clinical characteristics, aBMD, FRAX and HR-pQCT parameters in patients who experienced a new fragility fracture during the 5-year follow-up period (incident fracture group) were compared with patients who did not (control group).
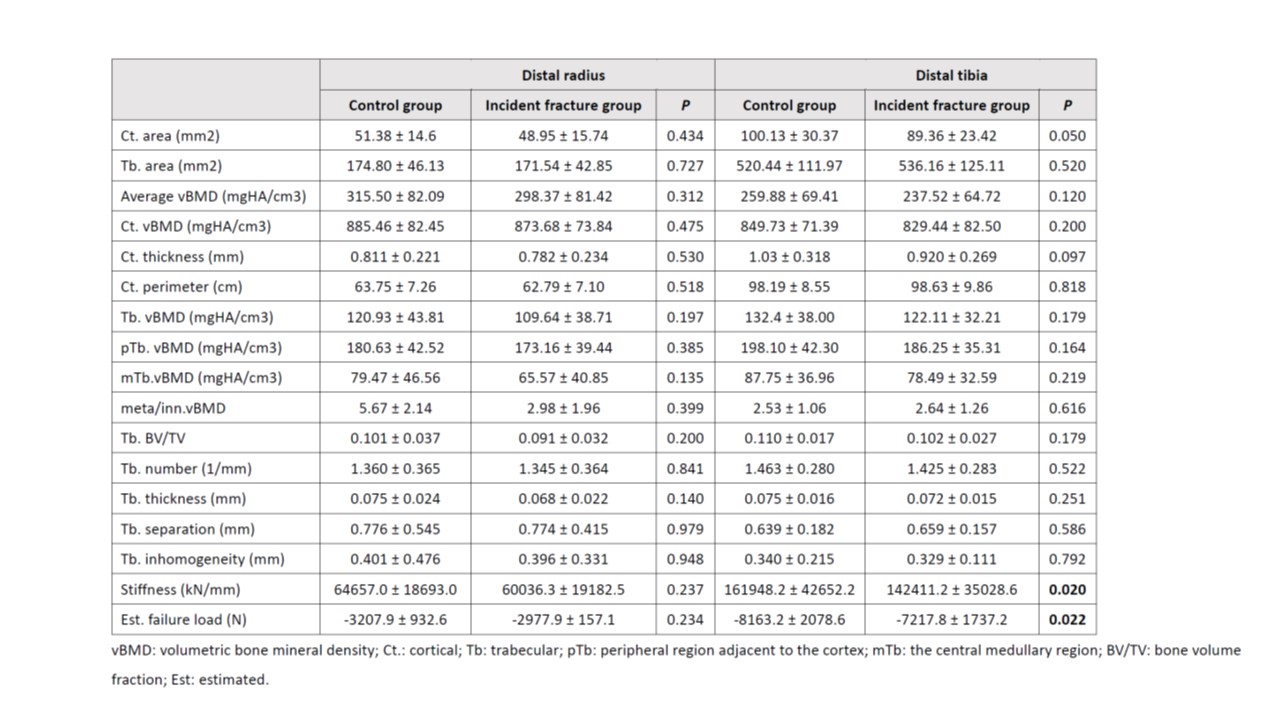
Results: In this interim analysis, a total of 109 patients were recruited. The mean age of the patients at the 5th year visit was 61.9 ± 12.2 years and there was a female predominance of 81.7%. Systemic lupus erythematosus (50.9%) and rheumatoid arthritis (21.3%) were the commonest rheumatological diagnoses. At baseline, 46.8% and 32.1% of the patients were osteopenic and osteoporotic respectively, 15.6% had a prevalent fracture. The baseline 10-year major osteoporotic and hip fracture risks by fracture risk assessment tool (FRAX) were 14.5 ± 13.7 and 6.5 ± 9.8 respectively. After 5 years, 35 (32.1%) of the patients developed new fractures (24 vertebral, 11 non-vertebral). The clinical characteristics of the incident facture group and the control group are shown in table 1. There was no difference in the aBMD and FRAX scores between the two groups. When comparing the HR-pQCT parameters, the incident fracture group had significantly lower tibial stiffness and failure load than the control group (table 2). Multivariate logistic regression confirmed that baseline bone stiffness (p=0.024) and failure load (p=0.026) over tibia were independent predictors of new fractures after adjusting for age, gender, prevalent fracture and osteoporosis status.
Conclusion: We conclude that impairment of bone strength over distal tibia on HR-pQCT predicts the occurrence of incident fracture in rheumatic disease patients on LTGC.
To cite this abstract in AMA style:
SO h, Lau X, Hung V, Pang S, Ying S, Kwok K, Lee K, Lee J, Lee J, Griffith J, Qin L, Tam L. Bone Microarchitecture Assessed by 3D High-resolution Peripheral Quantitative Computed Tomography (HR-pQCT) as Predictor of Incident Fracture in Rheumatic Disease Patients on Long-term Glucocorticoid- a Five-year Longitudinal Study [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/bone-microarchitecture-assessed-by-3d-high-resolution-peripheral-quantitative-computed-tomography-hr-pqct-as-predictor-of-incident-fracture-in-rheumatic-disease-patients-on-long-term-glucocorticoid/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/bone-microarchitecture-assessed-by-3d-high-resolution-peripheral-quantitative-computed-tomography-hr-pqct-as-predictor-of-incident-fracture-in-rheumatic-disease-patients-on-long-term-glucocorticoid/