Session Information
Date: Sunday, October 26, 2025
Title: (0233–0279) Miscellaneous Rheumatic & Inflammatory Diseases Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Behçet’s disease (BD) is a chronic systemic disease with heterogenous clinical presentations. The strongest genetic risk factor and diagnostic biomarker for BD is the class I major histocompatibility complex antigen HLA-B51. Although best studied in ‘Silk-Road’ populations, B51’s prevalence in BD varies considerably across different racial/ethnic groups (Capittini, et al. Dis Markers, 2021). The genetic risks in American populations with BD are limited. This study describes the associations between HLA-B alleles and demographics in a diverse BD population from a large urban academic medical center in Los Angeles County.
Methods: Inclusion criteria required that patients had HLA-B allele testing (by sequence-specific oligonucleotide-polymerase chain reaction typing) conducted in routine clinical care, and were identified as having BD with >2 ICD-9/10 codes for BD. A sensitivity analysis with a more restrictive cohort (>2 ICD-9/10 codes for BD, plus >1 rheumatology encounter, plus >1 DMARD prescription) was performed, and had similar demographic/genetic features. HLA-B alleles evaluated in the analysis included known relevant alleles (B51, B27), and the other 3 alleles of highest frequency.
Results: There were 144 identified BD patients, with B51 positivity in 33% (48 patients), versus a B51 prevalence of 11% among 2614 non-rheumatic controls (p< 0.0001). Amongst the BD patients, the alleles of highest frequency were B51 (49), B7 (31), B44 (28), and B35 (25) (Figure 1). Comparing B51(+) versus B51(-) BD patients, the groups were similar by age, gender, race/ethnicity and use of disease modifying agents (Table 1). However, there were higher percentages of B7(+) and B44(+) patients in the B51(-) group (Table 1). 35% of BD patients identified as white and compared to non-white BD patients had similar rates of B51(+), but a higher rate of B27(+) (16% vs 4%, p=0.01). White BD patients compared to white non-rheumatic controls had significantly higher B51(+) and B27(+). Non-white/Hispanic BD patients compared to non-white/Hispanic controls had significantly higher B51(+). The unadjusted odds ratios (OR) for BD (yes/no) demonstrated B51(+) 4.13 (95% CI 2.92, 5.85), female gender 3.5 (2.35, 5.30), and Hispanic ethnicity 0.48 (0.29, 0.77) (Figure 2). B51, gender, and Hispanic ethnicity remained significant in a multivariate model, and interaction terms were non-significant.
Conclusion: In a large diverse U.S. urban academic medical center, BD was significantly associated with B51(+) and was present in ~1/3 of BD patients. B51(+) did not differ significantly between race or ethnicity. White BD patients had significantly higher rates of B27(+) than non-rheumatic white controls, and non-white BD patients. This data shows that U.S. BD patients may have lower B51(+), and higher female prevalence than in Silk-Road BD populations, which may reflect different genetic/environmental risks for BD. Limitations include selection bias (patients had to have clinically indicated HLA-B allele testing), and misclassification bias utilizing ICD codes (though sensitivity analysis demonstrated similar baseline/genetic features).
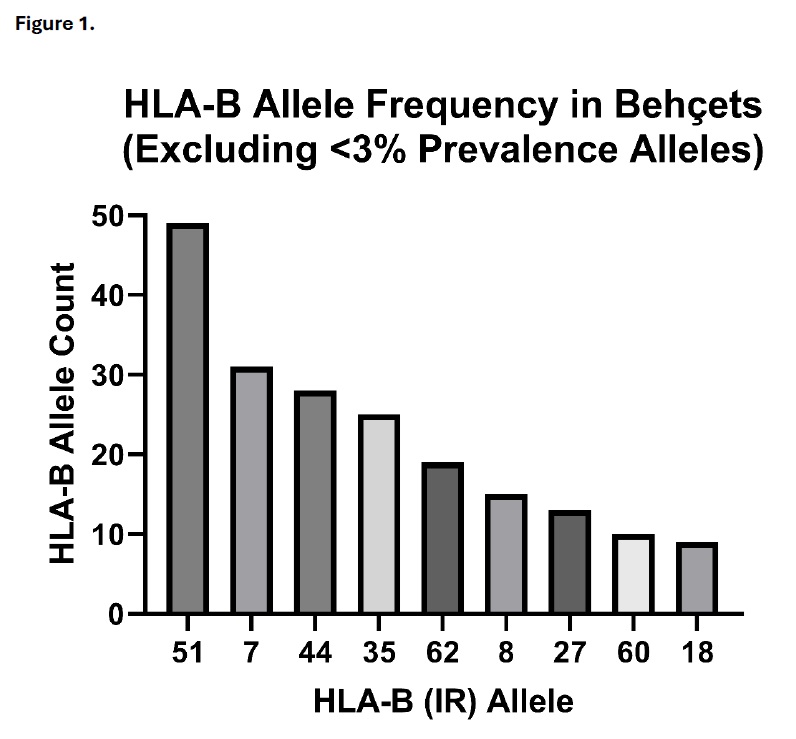 Values represent HLA-B allele count from total of 285 alleles (144 Behçet’s patients, 3 missing copies). Excluded the following HLA-B alleles representing < 3% prevalence, but still present at least once: HLA-B: 13, 37, 38, 39, 41, 42, 45, 46, 47, 48, 49, 50, 55, 56, 57, 58, 61, 63, 65, 67, 71, 72, 75, 77.
Values represent HLA-B allele count from total of 285 alleles (144 Behçet’s patients, 3 missing copies). Excluded the following HLA-B alleles representing < 3% prevalence, but still present at least once: HLA-B: 13, 37, 38, 39, 41, 42, 45, 46, 47, 48, 49, 50, 55, 56, 57, 58, 61, 63, 65, 67, 71, 72, 75, 77.
.jpg) Values represent n (%) for categorical variables, and mean (SD) for continuous variables.
Values represent n (%) for categorical variables, and mean (SD) for continuous variables.
Race, ethnicity, and gender are self-reported by the patient.
*p < 0.05, by Chi-Squared testing comparing B51(+) vs (-)
AAPI=Asian American/Pacific Islander, DMARD=disease modifying anti-rheumatic drug, csDMARD=conventional synthetic DMARD, bDMARD=biologic DMARD (RA=bDMARDs for RA, SpA=bDMARDs for spondyloarthritis, including IL17i, IL12/23i, IL23i), tsDMARD=targeted synthetic DMARD.
.jpg) Univariate logistic regressions for the outcome of Behçet’s Disease diagnosis.
Univariate logistic regressions for the outcome of Behçet’s Disease diagnosis.
To cite this abstract in AMA style:
Razmjou A, Klomhaus A, Kellner D, Fang M, Weisman M, FitzGerald J. Behçet’s Disease in a Diverse Urban Single-Center Cohort in the United States: HLA-B Alleles and Clinical Features [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/behcets-disease-in-a-diverse-urban-single-center-cohort-in-the-united-states-hla-b-alleles-and-clinical-features/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/behcets-disease-in-a-diverse-urban-single-center-cohort-in-the-united-states-hla-b-alleles-and-clinical-features/
