Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Infective Endocarditis (IE) is an important mimic of numerous forms of systemic vasculitis and especially Anti-Neutrophilic Cytoplasmic Antibody vasculitis (AAV). Bartonella endocarditis (BE) is the leading culture negative endocarditis, leading to missed diagnosis even in patients screened with blood cultures. BE causes multiple clinical features that overlap with AAV including Glomerulonephritis (GN). ANCA positivity has been reported in upwards of 60-75% of cases of BE. BE associated renal pathologic descriptions are heterogeneous, most often revealing vary degrees of immune complex GN and more rarely pauci-immune GN.
Critically if BE is missed and immunosuppression is given for presumed AAV, the outcomes can be fatal. The goal of the current study is to analyze all cases of BE associated GN at our institute and describe laboratory findings to potentially better recognize BE cases and reduce potentially fatal missed diagnosis.
Methods: A systemic search of our health systems EMR for hospitalized patients including with positive Bartonella Henselae Antibody titer IgG or “Bartonella Infection.” Definitive diagnosis of Bartonella was made if valvular histology demonstrated either positive Warthin Starry staining or Bartonella PCR. Probable Bartonella diagnosis was made with high titer serum Bartonella IgG ( >1:256) or Bartonella PCR blood positivity in combination with abnormalities seen on echocardiogram. Besides the diagnosis of BE, patients also required evidence of GN. GN was considered definitive if consistent renal histopathology was available. GN was considered probable with new onset acute kidney injury and microscopic hematuria at the time of Bartonella diagnosis. Patients who fulfilled definitive or probable BE and definitive or probable GN were included in the cohort. Multiple data points were collected including autoimmune serologies. Thrombocytopenia was defined as a platelet count of less than 150 k/uL, leukopenia defined as a white blood cell less than 3.70 k/uL at any point during their hospitalization.
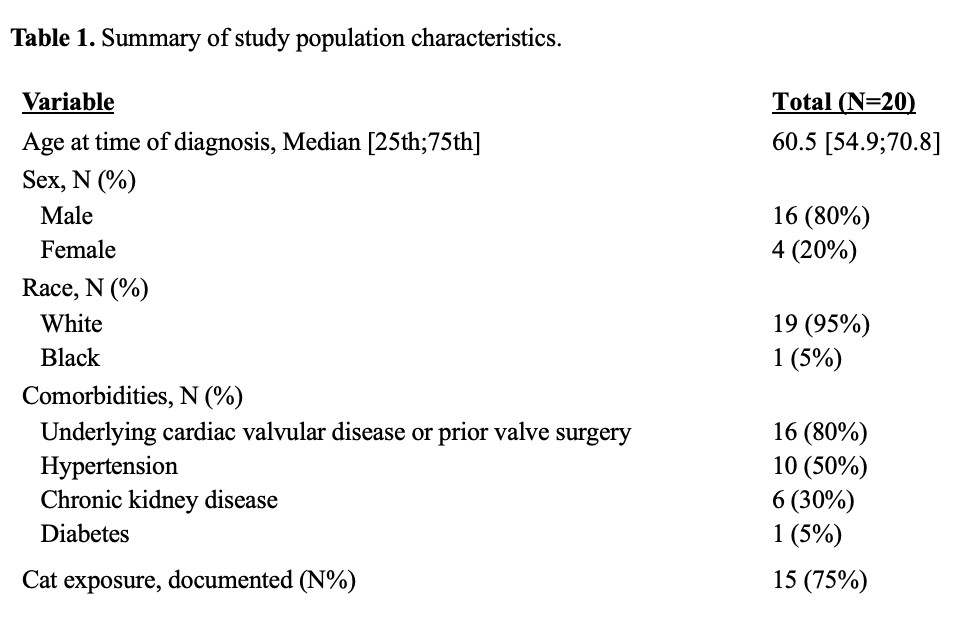
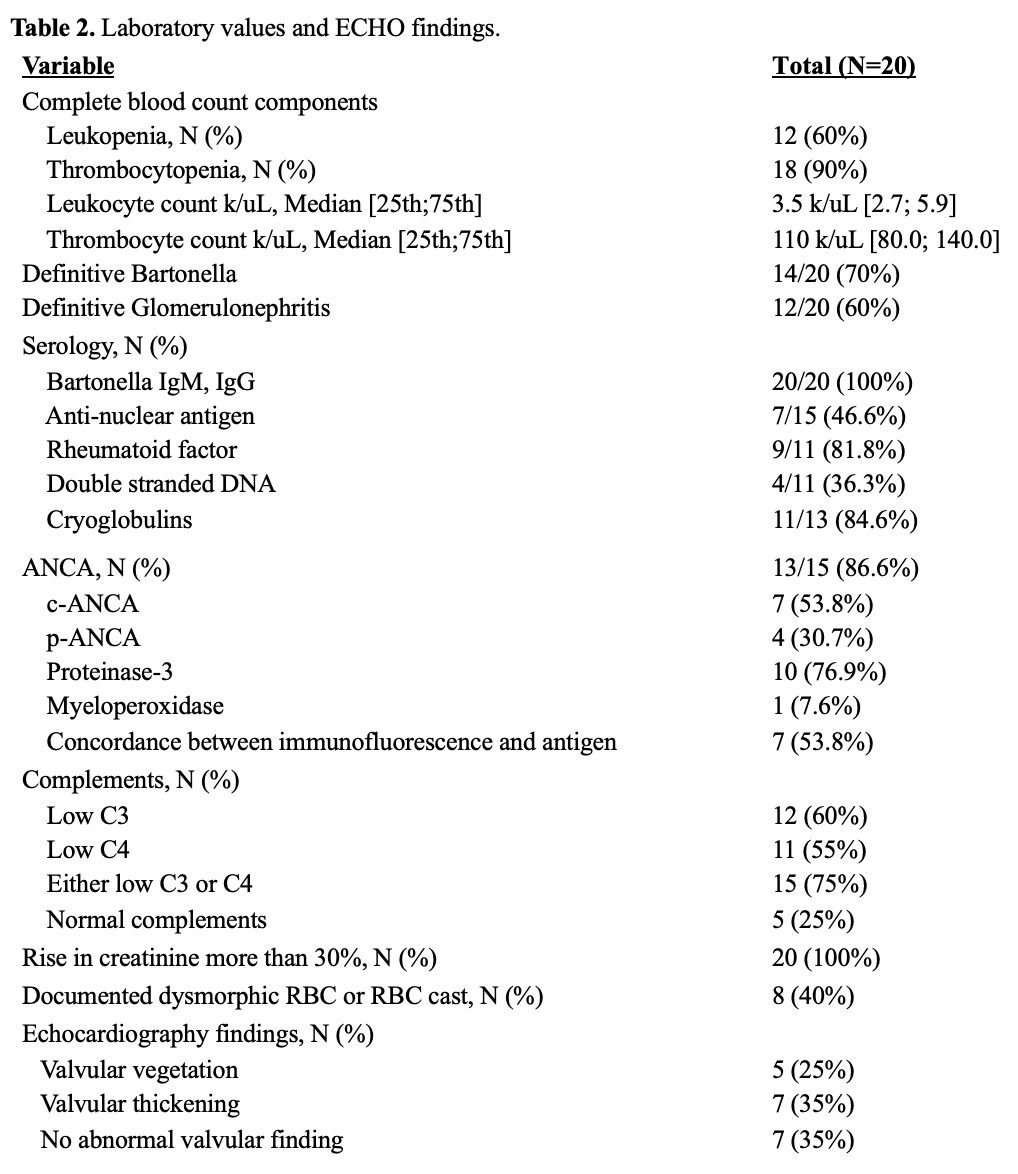
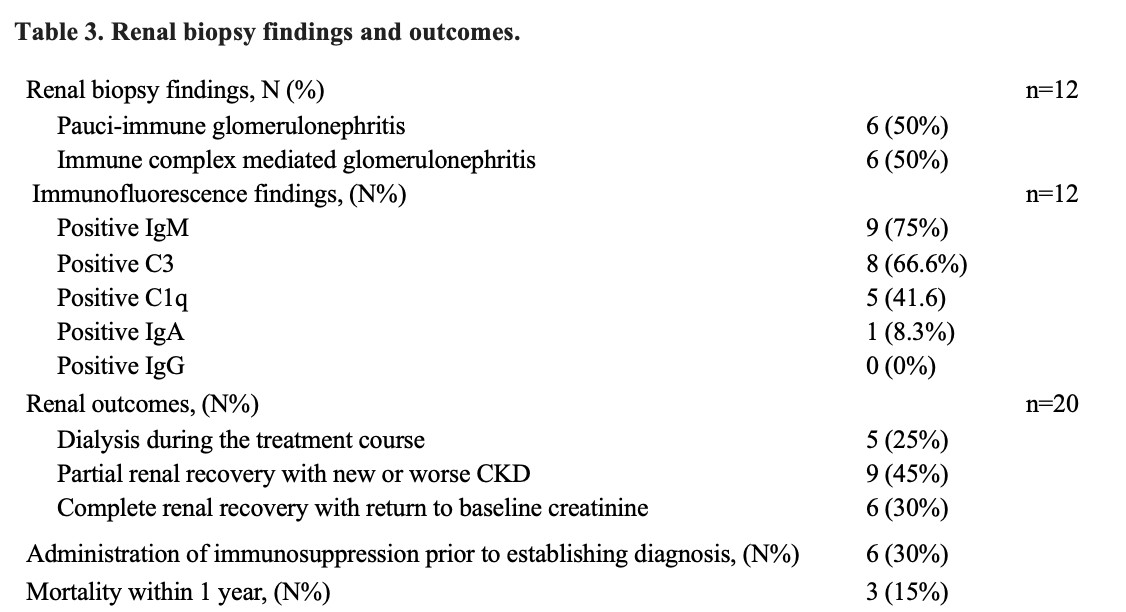
Results: 20 patients with BE were included in this cohort. 80% had known underling cardiac valve disease (Table 1). During initial hospitalization, 90% of patients had thrombocytopenia, 60% leukopenia and ANCA was detected in 87% of cases when checked. Either C3 or C4 were low in 75% of cases. Only 25% of echocardiograms revealed vegetations (Table 2). Renal histology was considered Pauci-Immune in 50% of cases (Table 3).
Conclusion: BE is an important mimic of AAV. Even when the diagnosis of endocarditis is being considered, Bartonella can be missed as it’s typically culture negative and only a minority of echocardiograms demonstrated vegetations. We present the largest single-center cohort of BE with GN. ANCA positivity was higher than in other cohorts at 87% as well our cohort had higher rates of (50%) of pauci-immune GN. The majority of echocardiograms did not reveal features considered specific for endocarditis such as vegetations. Of note, 90% of cases had thrombocytopenia at presentation as well as the majority (75%) had low serum complements both atypical features for primary AAV and should prompt further investigation for secondary causes of ANCA positivity.
To cite this abstract in AMA style:
Brown A, Vural A, Calabrese C, Calabrese L. Bartonella Endocarditis as an Important Mimic of ANCA Associated Vasculitis: Results of a Large Single Center Descriptive Analysis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/bartonella-endocarditis-as-an-important-mimic-of-anca-associated-vasculitis-results-of-a-large-single-center-descriptive-analysis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/bartonella-endocarditis-as-an-important-mimic-of-anca-associated-vasculitis-results-of-a-large-single-center-descriptive-analysis/