Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose:
It is known that patients diagnosed with axSpA do not subsequently meet the classification criteria. The Objectives are: To estimate the diagnostic prevalence of axSpA in patients who started low back pain over 45 years of age and to analyze the clinical, laboratory and imaging differences with patients who started it before that age.
Methods:
Methods: Observational and cross-sectional study, which included patients older than 18 years with a diagnosis of axial spondyloarthritis performed between 2017 and 2021. At baseline, all patients underwent: blood tests, HLA B27, X-rays and MRI of the sacroiliac joint, enthesis ultrasound, sociodemographic data, level of education and habits were also recorded. Axial spondyloarthritis symptoms, age of onset, delay to diagnosis, characteristics of low back pain, characteristics of axial spondyloarthritis, NSAIDs intake and response, VAS pain and night pain, morning stiffness time. In addition, BASDAI, BASFI, MASES and HAQ scores were used. The symptom evaluator was unaware of the results of the complementary studies that were collected by another observer. The MRIs recorded the presence of any lesion and classified it into acute (edema) and chronic (fatty changes, erosions, sclerosis, and bone bridges) lesions.
Results:
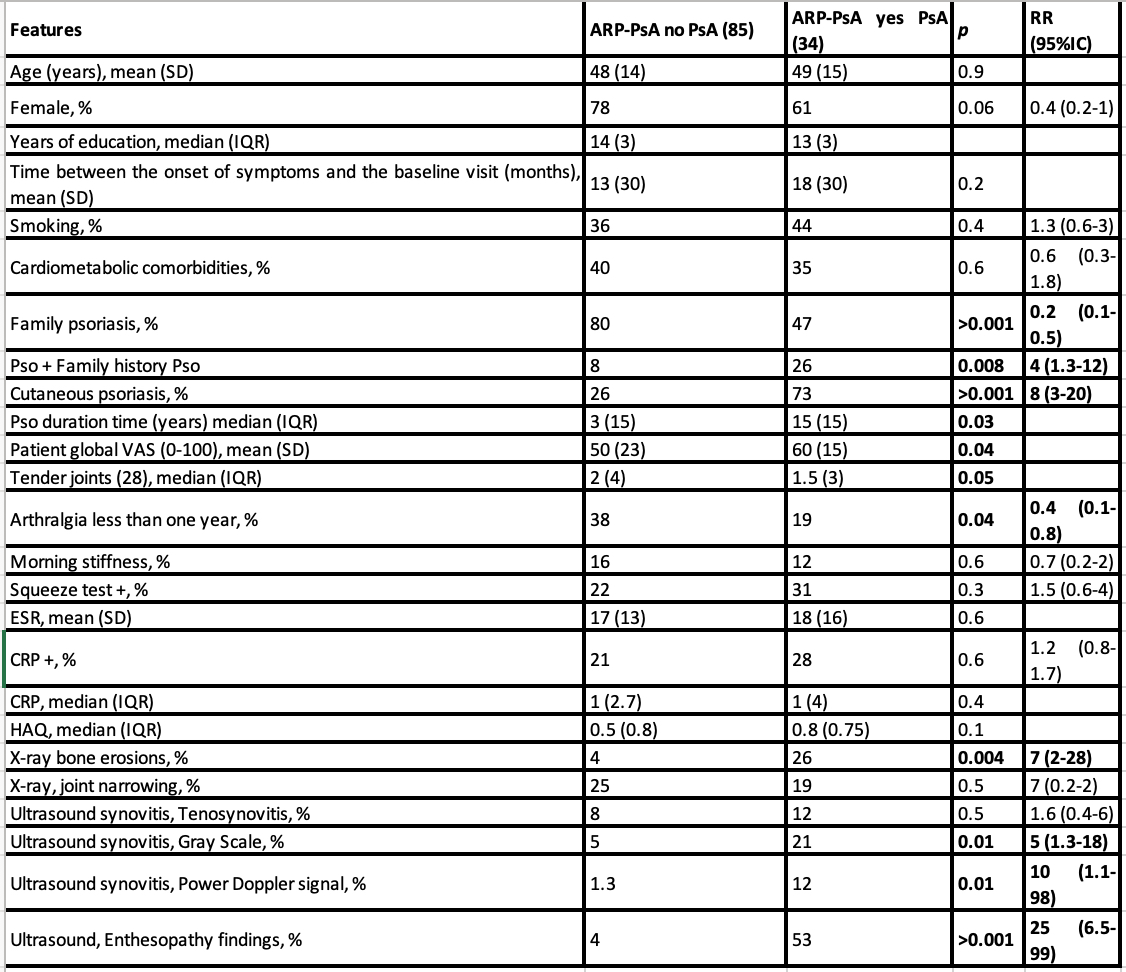
Results: One hundred sixteen patients with a diagnosis of axial spondyloarthritis were included, whose characteristics are summarized in Table 1. The prevalence of patients who started low back pain after the age of 45 was 31.28% (95% CI 20-36 ). The relevant differences were: female sex (51% vs 29% p 0.03), smoking (38% vs 57% p 0.07), psoriasis (42% vs 17% p 0.007), good response to NSAIDs (52% vs 73% p 0.03), HLA-B27 (+) (32% vs %54 p 0.04), more than 4 characteristics of axial spondyloarthritis (35% vs 54% p 0.08), BASFI (5.1 vs 4.5 p 0.05), delay to diagnosis in months (40 vs 93 p 0.002). No differences were found in terms of disease activity and imaging (MRI or X-rays). In the logistic regression analysis, the variables that were independently associated were: male sex (OR 0.2 IC95% 0.06- 0.8), psoriasis (OR 4.8 IC95% 1.1-29), and shorter delay to diagnosis (OR 0.9 IC95% 0.96 -0.99).
Conclusion: The prevalence of diagnosis of axial spondyloarthritis in patients who started low back pain after the age of 45 was 28%. The characteristics of these patients were: female sex, higher frequency of psoriasis, and shorter delay to diagnosis. This study shows that the older age at the onset of low back pain and the association with psoriasis could show a group of patients with axial involvement in the context of psoriatic disease.
To cite this abstract in AMA style:
garcía salinas r, Reyes G, Jaldín Céspedes R, Almada F, Magri S. Axial Spondyloarthritis in Patients with Late-Onset Chronic Low Back Pain (Older Than 45 Years). Axial Spa or Psoriatic Disease with Axial Involvement? [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/axial-spondyloarthritis-in-patients-with-late-onset-chronic-low-back-pain-older-than-45-years-axial-spa-or-psoriatic-disease-with-axial-involvement/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/axial-spondyloarthritis-in-patients-with-late-onset-chronic-low-back-pain-older-than-45-years-axial-spa-or-psoriatic-disease-with-axial-involvement/