Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Primary Antiphospholipid Syndrome (PAPS) patients, when submitted to Systemic Lupus Erythematosus (SLE) classification criteria, can be misclassified. The new 2019 ACR/EULAR classification criteria have never been applied for PAPS patients. The main objective of this study is to evaluate the risk of misclassifying thrombotic PAPS (Sidney) as SLE in a cohort of a tertiary Hospital.
Methods: A retrospective analysis of our PAPS cohort was performed using electronic chart database. The three current classification criteria for SLE (ACR 1997, SLICC 2012 and 2019 ACR/EULAR) were applied in parallel focusing on the latter. Flowchart of the study is shown in Figure 1. Categorical variables were analyzed by x2 or two-tailed Fisher’s exact test, and continuous variables were analyzed by Student’s T test or Mann–Whitney-U test, as applicable. The misclassification rates of the three different criteria were compared using McNemar’s test. A p-value of < 0.05 was considered statistically significant.
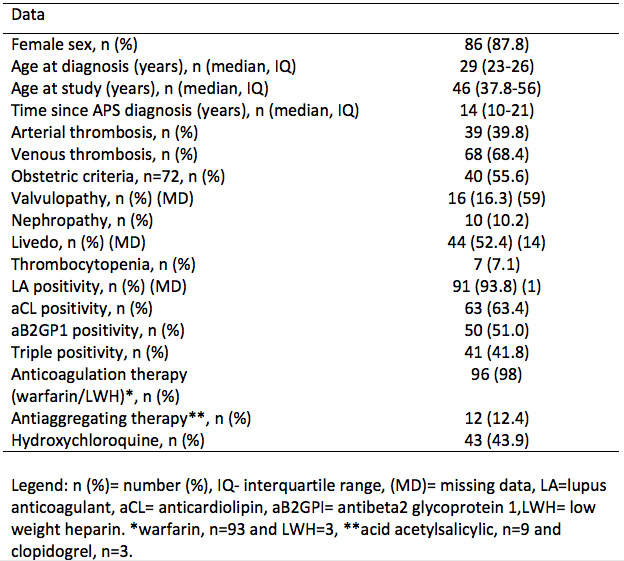
Results: All patients had thrombotic PAPS and 55.6% presented obstetric criteria manifestations. Venous and arterial thrombosis were detected in 69.4% and 39.8%, respectively. Ninety-eight PAPS patients were submitted to ACR 1997 and 2019 ACR/EULAR. SLICC 2012 was applied in only 83 patients due to missing data (lack of direct Coombs test). Our patients were mostly female (87.8%), with a median age at study inclusion of 46 years (38-56) and median disease duration of 14 years (10-21). LA was the most frequent antiphospholipid antibody, identified in 91 patients (93.8%). Main characteristics of the studied patients are shown in Table 1. The comparison of different criteria two-by-two according to their rates of misclassification found that 2019 ACR/EULAR and ACR 1997 performed similarly (N=98; 6.1 vs. 6.1%, p=1.00). On the other hand, SLICC 2012 demonstrated a poor performance compared to both 2019 ACR/EULAR (N=83, 36.1 vs. 6.1%, p< 0.001) and ACR 1997 criteria (N=83, 36.1 vs. 6.1%, p< 0.001). When the 3 classification criteria were used simultaneously, only 1 patient was misclassified as SLE. Hematological manifestations were the most frequent criteria related to misclassification in PAPS patients, encompassing 100% of misclassified patients (vs. 52.2%, p=0.025) in ACR 1997, 90% (vs. 11.3%, p< 0.001) in SLICC 2012 and 71.4% (vs. 18.6%, p=0.01) in 2019 ACR/EULAR.
Conclusion: 2019 ACR/EULAR is very accurate in differentiating PAPS from SLE, with only 6.1% of misclassification rates (similar to those observed in ACR 1997 and lower than those found in SLICC 2012).
To cite this abstract in AMA style:
Signorelli F, Balbi G, Bonfa E, Borba E, Andrade D. Avoiding Misclassification of Primary Antiphospholipid Syndrome as Systemic Lupus Erythematosus: What Are the Best-performing SLE Classification Criteria? [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/avoiding-misclassification-of-primary-antiphospholipid-syndrome-as-systemic-lupus-erythematosus-what-are-the-best-performing-sle-classification-criteria/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/avoiding-misclassification-of-primary-antiphospholipid-syndrome-as-systemic-lupus-erythematosus-what-are-the-best-performing-sle-classification-criteria/