Session Information
Date: Sunday, November 10, 2019
Title: 3S089: Health Services Research I: Clinical Perspectives (951–956)
Session Type: ACR/ARP Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: Nearly 25% of patients with SLE are hospitalized each year often for outcomes that may have been avoided if patients had received sustained, high quality outpatient care. A recent Delphi panel defined SLE-specific adverse outcomes that may result in avoidable acute care use (emergency department [ED] visits or hospitalizations) and included 7 vaccine-preventable illnesses. We used U.S. nationwide data from a vulnerable SLE population to describe the burden of acute care use for these illnesses and to examine demographic and healthcare utilization predictors.
Methods: Using claims data from Medicaid (public insurance for low income individuals) from 29 U.S. states (2000-2010), we identified adults (18-65 years) with prevalent SLE (≥3 ICD-9 codes 710.0 separated by ≥30 days). We required 12 months of enrollment prior to the first code (index date) to identify baseline comorbidities, vaccine uptake, and healthcare utilization. We defined avoidable acute care use for vaccine-preventable illnesses as discharge diagnosis codes from ED visits or hospitalizations for influenza, pneumococcal disease, meningococcal disease, herpes zoster, high-grade cervical dysplasia/cervical cancer, and hepatitis B, after the index date. We estimated the incidence rate (IR) of acute care use for vaccine-preventable illnesses and used Cox regression to assess risk (HR, 95% CI) of first acute care visit for vaccine-preventable illnesses by baseline demographics and healthcare use, adjusting for vaccinations, SLE-related comorbidities and medications.
Results: We identified 46,075 Medicaid beneficiaries with SLE with mean follow-up of 4 (SD 3) years. The mean age was 39 (SD 12) and 93% were female, 40% were black, 38% white, 13% Hispanic, 2% Asian. Vaccine uptake during the 12-month baseline period included: 3,331 (7.2%) receiving the influenza vaccine, 1,020 (2.2%) shingles, 551 (1.2%) pneumococcal, 290 (0.63%) hepatitis B, 91 (0.2%) human papillomavirus, and 17 (0.04%) meningitis. The incidence rate of acute care use for vaccine-preventable illnesses was 6.8 per 1,000 person-years; most were herpes zoster, influenza or pneumococcal disease (Table 1). 93% of events occurred in patients who had not received baseline vaccinations. In adjusted analyses, we observed a higher risk of acute care use for vaccine-preventable illnesses among black patients, in the Midwest and South, and among patients with more baseline ED visits and hospitalizations (Table 2). Greater outpatient visits were associated with a dose-response reduction in acute care use, with >30% reduced risk (HR 0.69, 95% CI 0.56-0.74) comparing >10 visits to none.
Conclusion: Claims for vaccinations in this nationwide, vulnerable population of SLE patients were rare, likely reflecting a combination of underreporting and low uptake. As expected, patients with vaccine claims had minimal acute care use for vaccine-preventable illnesses. Greater outpatient use was associated with significantly reduced risk of ED visits and hospitalizations for vaccine-preventable illnesses suggesting that established, consistent outpatient care with optimal SLE monitoring and management, and access to preventive care, can reduce avoidable acute care use.
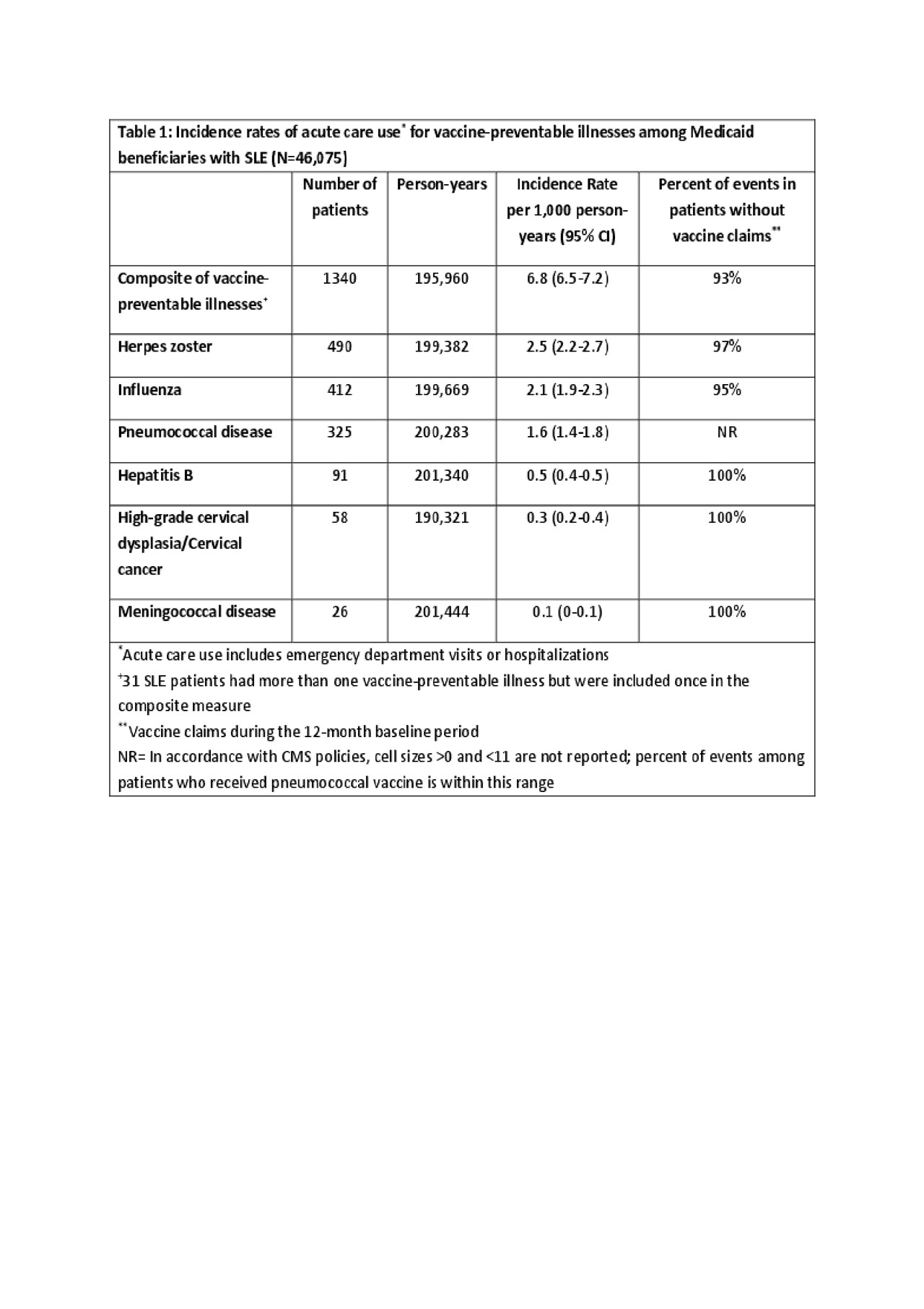
Table 1 Vaccine Prevent Illness ACR
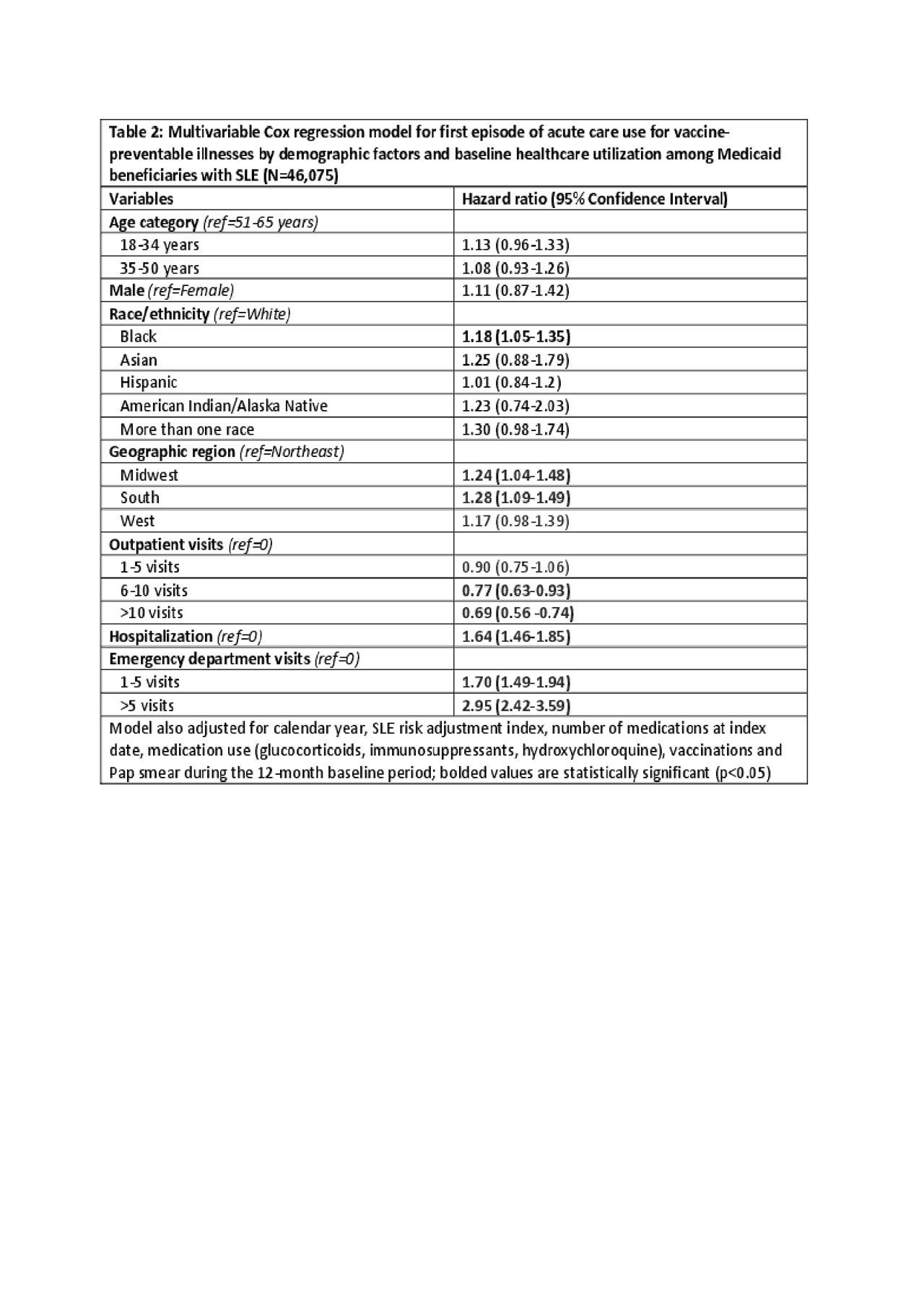
Table 2 Avoidable vaccine abstract
To cite this abstract in AMA style:
Feldman C, Xu C, Costenbader K. Avoidable Acute Care Use for Vaccine-Preventable Illnesses Among Medicaid Beneficiaries with Lupus: Demographic and Healthcare Utilization Differences [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/avoidable-acute-care-use-for-vaccine-preventable-illnesses-among-medicaid-beneficiaries-with-lupus-demographic-and-healthcare-utilization-differences/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/avoidable-acute-care-use-for-vaccine-preventable-illnesses-among-medicaid-beneficiaries-with-lupus-demographic-and-healthcare-utilization-differences/
