Session Information
Date: Monday, November 18, 2024
Title: SLE – Treatment Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: For patients with SLE who are treated with glucocorticoids (GC), discontinuation of the latter is an important goal. However, the clinical conditions under which this can be safely achieved without increasing the risk for exacerbation remain ill-defined, particularly in cases of moderate to severe disease activity. We aimed to discern factors associated with the risk for flare in SLE patients who discontinued GC.
Methods: Retrospective cohort study of 384 adult SLE patients with moderate-to-severely active disease at entry (SLEDAI- 2K ≥6 and/or PGA ≥1.5, requiring treatment intensification with ≥20 mg/day prednisone equivalent and/or initiation with immunosuppressive or biological agent), with 5 years median follow-up. Survival analysis methods, encompassing Kaplan-Meier (KM) estimation and Cox regression, and generalized linear models were employed to explore the risk for flares (SELENA-SLEDAI flare index) following GC withdrawal, in relation to attainment of remission (DORIS) or low disease activity state (LLDAS), time spent in remission, concomitant use of immunomodulatory/-suppressive agents, and speed of GC tapering.
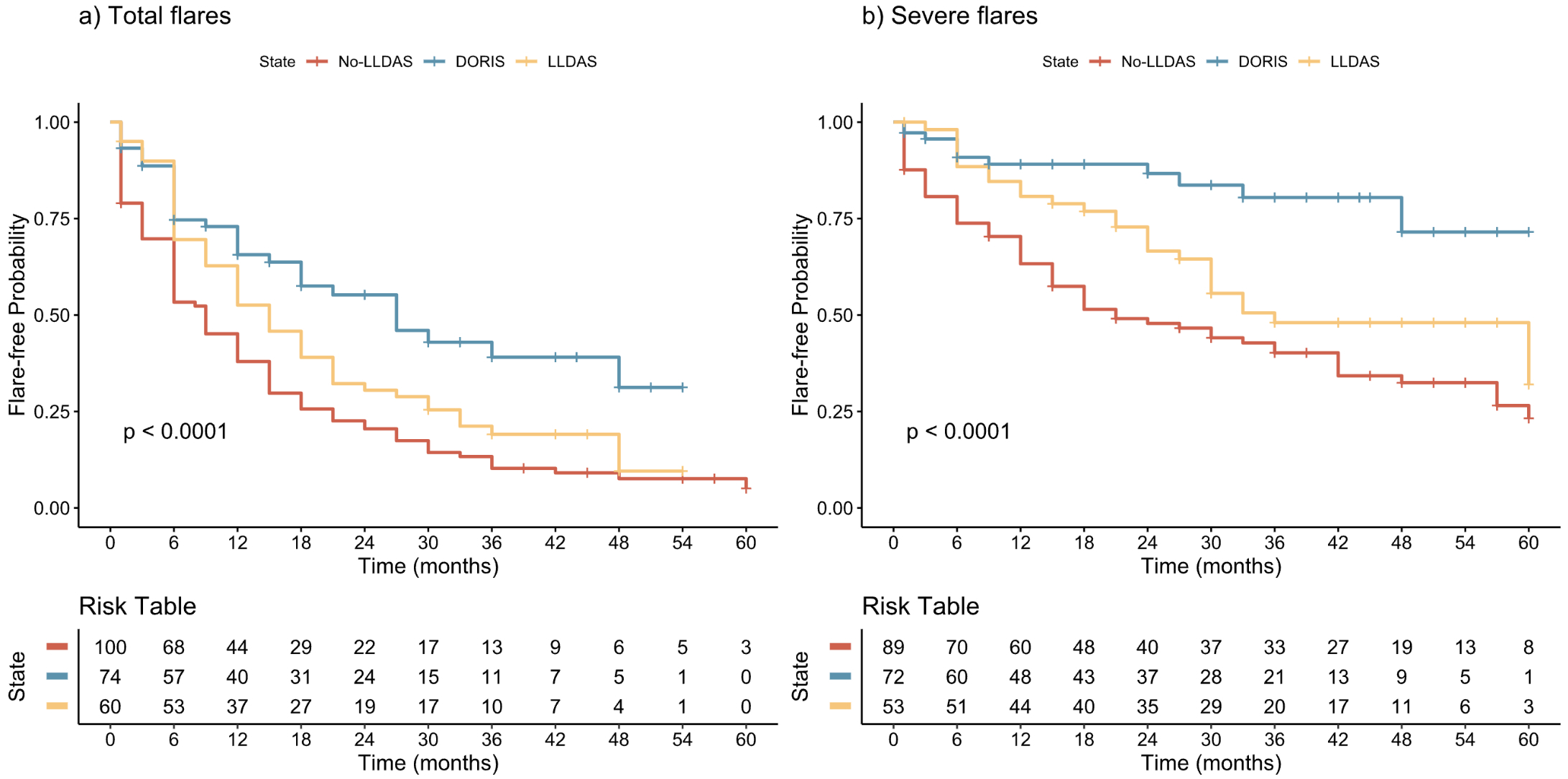
Results: During follow-up, 71% of patients discontinued GC at least once. Following discontinuation, the KM-estimated risk of flares and severe flares at 6, 12, and 24 months was 0.35, 0.50, and 0.67, and 0.15, 0.22, and 0.32, respectively. Being in LLDAS or DORIS at the time of GC withdrawal was protective against subsequent flares, with hazard ratios (HRs) of 0.71 (95% CI 0.50-1.01) and 0.41 (95% CI 0.28-0.61), respectively (Figure 1). An 11% reduction in flare risk (P < 0.001) was observed for every three months duration of remission prior to GC withdrawal. Hydroxychloroquine use was associated with a lower risk of severe flares (HR: 0.50, 95% CI: 0.33-0.75), while mycophenolate mofetil (MMF) and azathioprine (AZA) significantly reduced the risk of total –but not severe– flares (HRs: 0.32, 95% CI: 0.13-0.79 and 0.48, 95% CI: 0.31-0.75, respectively). Furthermore, the speed of GC tapering was correlated with subsequent flare risk; patients in whom tapering from 7.5 mg/day prednisone equivalent to complete withdrawal was delayed for more than three months had lower risks for both total and severe flares (HRs 0.69, 95% CI: 0.50-0.95, and 0.61, 95% CI: 0.38-0.97), respectively, and this effect was independent of concurrent use of immunosuppressives. A risk-benefit analysis revealed that, in patients who discontinued GC, the increased risk for flares (incidence rate ratio [IRR]: 1.65, 95% CI: 1.38-1.98, versus patients who continued GC) and severe flares (IRR: 1.52, 95% CI: 1.16-2.01), was counterbalanced by a reduced risk for organ damage accrual (IRR: 0.37, 95% CI: 0.25-0.55).
Conclusion: A low disease activity or remission state, together with concurrent use of hydroxychloroquine and immunosuppressives, along with a gradual tapering tempo provides a relatively safer clinical context to attempt GC discontinuation in SLE.
To cite this abstract in AMA style:
Katechis S, Pitsigavdaki S, Nikoloudaki M, Garantziotis P, Silvagni E, Repa A, Marangoni A, Flouri I, Avgoustidis N, Parperis K, Govoni M, Sidiropoulos P, Boumpas D, Fanouriakis A, Bertsias G, Bortoluzzi A. Attainment of Remission, Use of Immunomodulatory/suppressive Agents and Gradual Dose Tapering May Facilitate Flare-free Withdrawal of Glucocorticoids in Patients with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/attainment-of-remission-use-of-immunomodulatory-suppressive-agents-and-gradual-dose-tapering-may-facilitate-flare-free-withdrawal-of-glucocorticoids-in-patients-with-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/attainment-of-remission-use-of-immunomodulatory-suppressive-agents-and-gradual-dose-tapering-may-facilitate-flare-free-withdrawal-of-glucocorticoids-in-patients-with-systemic-lupus-erythematosus/