Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Cigarette smoke is a known inhalant exposure that contributes substantially to the risk and severity of rheumatoid arthritis (RA). Less is known about the link between other inhalant exposures and RA related factors. The aim of this study was to determine the association between inhalant exposures (occupational, agricultural, and military) with RA-related autoantibodies and severity in U.S. Veterans with RA.
Methods: Participants at 9 sites in the Veterans Affairs Rheumatoid Arthritis (VARA) Registry, a multicenter, longitudinal observational cohort of U.S. Veterans with RA, were mailed surveys assessing occupational, agricultural, and military inhalant exposures. Demographics, disease activity, functional status, and extra-articular features were obtained from the VARA registry database while HLA-DRB1 shared epitope (SE) status, anti-CCP antibodies, and rheumatoid factor (RF) were measured using banked serum from VARA enrollment. Cross sectional associations between self-reported inhalant exposures and RA-related factors (autoantibodies, severity, extra-articular features) were assessed using multivariable linear and logistic regression models adjusting for age, sex, race, and tobacco use. Associations between inhalant exposures and autoantibody status were further examined in models stratified by SE status.
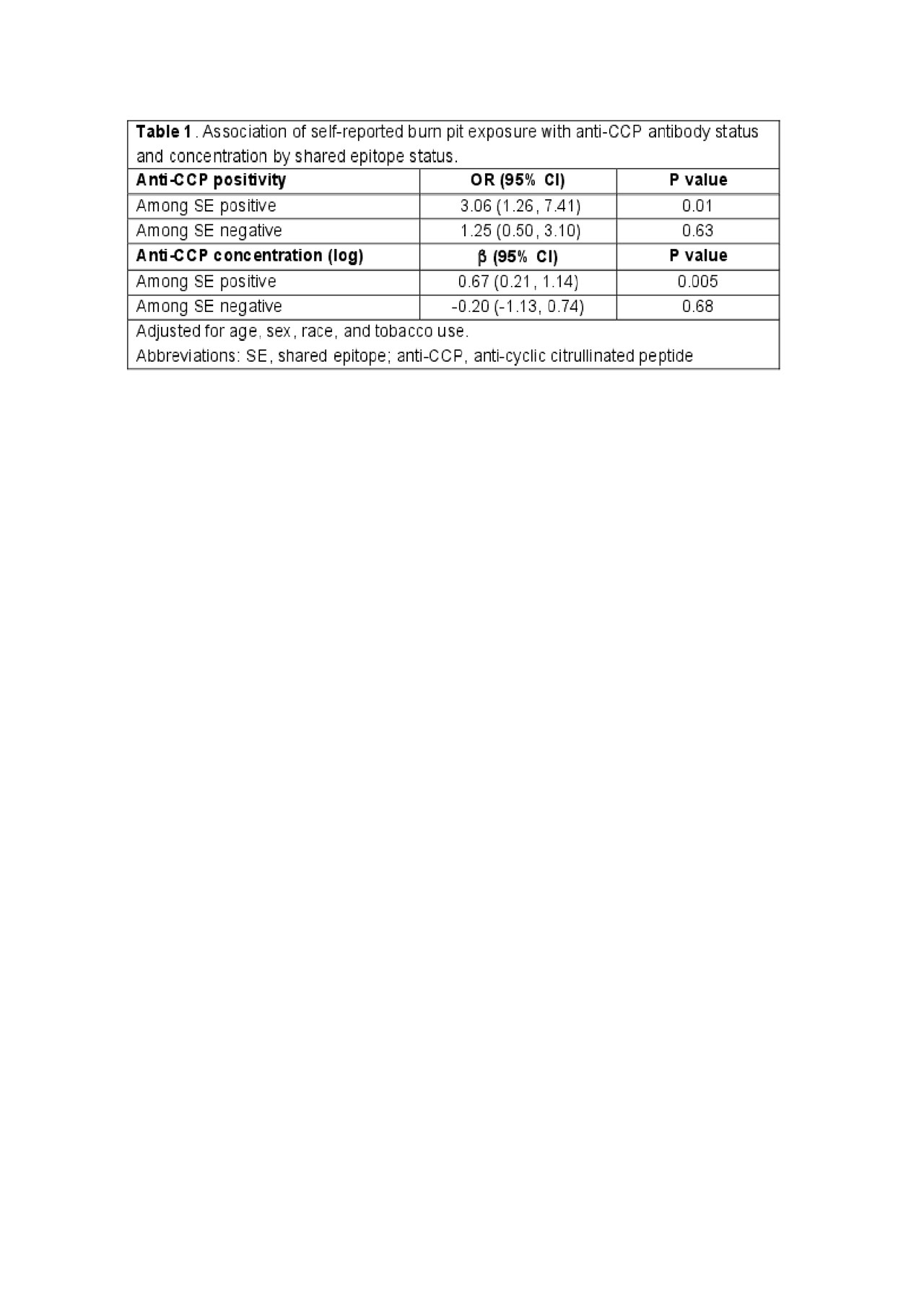
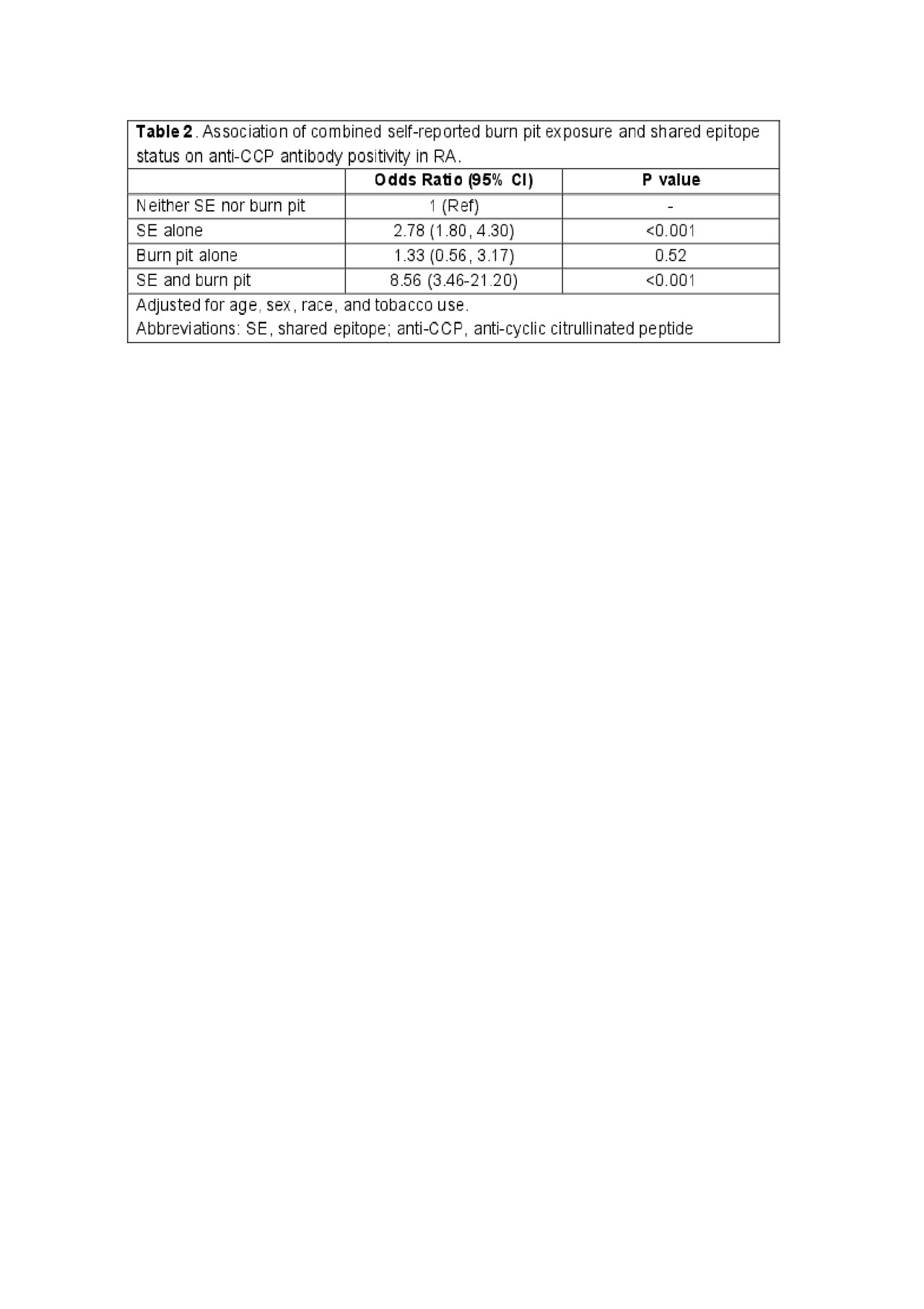
Results: Of 1566 registry participants mailed surveys, 797 returned completed surveys (50.9% response rate). Responders were older, more frequently white, less frequently current smokers, and had better disease activity and functional status. Self-reported occupational dust exposures were present in 67.6%, living or working on a farm in 44.8%, Agent Orange exposure in 29.2%, and military burn pit exposure in 18.6%. Military service periods between 1965-1973 were most common among those self-reporting burn pit exposure, with 19% serving during periods characterized by open-air burn pits on military bases. There were no significant associations between occupational dust, farm, or Agent Orange exposures with RA autoantibodies or disease severity. Self-reported burn pit exposure was significantly associated with anti-CCP positivity (odds ratio [OR] 2.22, 95% CI 1.23-3.99) and higher anti-CCP concentrations (log-transformed; b0.50, 95% CI 0.07-0.93) independent of tobacco use. In analyses stratified by SE status, these associations were limited to individuals with SE alleles (Table 1). In models examining combined self-reported burn pit exposure and SE status, those with both risk factors demonstrated a substantially higher risk of anti-CCP positivity (OR 8.56, 95% CI 3.46-21.20) compared to either risk factor in isolation (Table 2). Self-reported burn pit exposure was not associated with RF positivity, disease activity, or extra-articular disease.
Conclusion: Self-reported burn pit exposure was associated with anti-CCP antibodies in those with HLA-DRB1 SE alleles independent of, and to a similar degree as tobacco use. While limited by the cross-sectional design and self-report exposure history, these findings suggest that other inhalant exposures may similarly influence RA autoantibody expression and confer risk for RA
To cite this abstract in AMA style:
Ebel A, Poole J, Thiele G, Baker J, Cannon G, Gaffo A, Kerr G, Reimold A, Richards J, Schwab P, Singh N, Ascherman D, Mikuls T, England B. Associations of Self-Reported Inhalant Exposures with Autoantibodies and Disease Severity in U.S. Veterans with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/associations-of-self-reported-inhalant-exposures-with-autoantibodies-and-disease-severity-in-u-s-veterans-with-rheumatoid-arthritis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/associations-of-self-reported-inhalant-exposures-with-autoantibodies-and-disease-severity-in-u-s-veterans-with-rheumatoid-arthritis/