Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Mental health disorders, including depression, anxiety, and post-traumatic stress disorder, are prevalent among people with SLE. In other disease populations, these disorders have been associated with increased acute care use. We quantified the association between mental health conditions and recurrent acute care use (emergency department [ED] visits, hospitalizations) among patients with SLE.
Methods: We used data from the nationwide All of Us Research Program (version 8), an NIH cohort of >393,000 U.S. adults who enrolled and consented for linkage to their electronic health records. We identified those with >2 ICD-10 or SNOMED codes for SLE in the 2 years pre-enrollment. We assessed for mental health diagnoses in that time, identified by ≥2 ICD-10 or SNOMED codes for major depression, anxiety, or PTSD. The outcome was number of emergency department visits (only) and hospitalizations (including from emergency department) after enrollment. Incidence rates for acute care use among patients with and without mental health diagnoses were calculated. Multivariable negative binomial regression models calculated incidence rate ratios (IRRs), adjusting for age, sex, race, ethnicity, enrollment year, baseline sociodemographic factors and comorbidities.
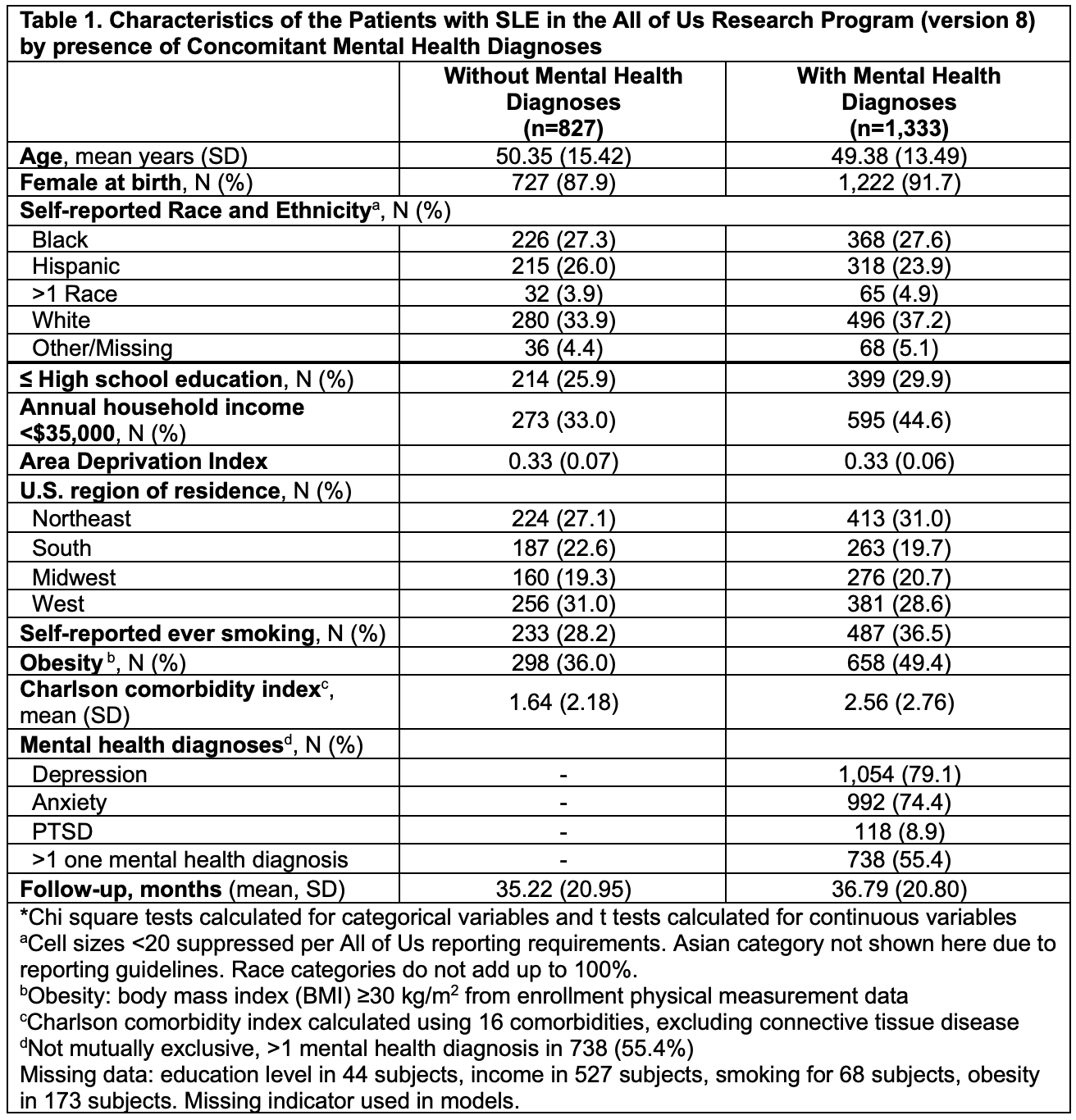
Results: We identified 2,160 with SLE, of whom 1,333 (61.7%) had depression, anxiety, and/or PTSD (Table 1). Mean age overall was 49.8 (14.3) and 90.2% were female. Those with ≥1 mental health condition were more likely to be less educated, in a low-income group, to have ever smoked, and to have more comorbidities. Patients were followed for a mean 36.2 months (SD 20.9) after enrollment. Incidence rates for all acute care were much higher in those with mental health disorders (Table 2). In adjusted analyses (Table 2), we found strong associations between having mental health diagnoses and higher rates of acute care use, both emergency department visits (adj IRR 2.12, 95%CI 1.79-2.52) and hospitalizations (adj IRR 1.95, 95%CI 1.59-2.41). This was true both for all emergency visits and hospitalizations for SLE (adj IRR 1.80, 95%CI 1.50-2.16) and for all diagnoses (adj IRR 1.92, 95% CI 1.60, 2.30).
Conclusion: In this large US-wide population of patients with SLE, mental health diagnoses were extremely prevalent and those with them had much higher rates of recurrent acute care use compared to those without these diagnoses. As patients with frequent acute care use are less likely to receive standard-of-care long-term medications and preventive care, contributing to inequities, further work is needed to develop interventions to decrease this recurrent acute care use for patients with SLE and mental health disorders.
To cite this abstract in AMA style:
Costenbader K, Yee J, Guan H, Oakes E, Cui J, Santacroce L, Karlson E, Koenen K, Kubzansky L, Feldman C. Associations Between Mental Health Diagnoses and Acute Care Use Among Individuals with Systemic Lupus Erythematosus in the All of Us Research Program [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/associations-between-mental-health-diagnoses-and-acute-care-use-among-individuals-with-systemic-lupus-erythematosus-in-the-all-of-us-research-program/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/associations-between-mental-health-diagnoses-and-acute-care-use-among-individuals-with-systemic-lupus-erythematosus-in-the-all-of-us-research-program/

.jpg)