Session Information
Date: Saturday, November 6, 2021
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster I: Diagnosis (0323–0356)
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: Systemic lupus erythematosus (SLE) and myasthenia gravis (MG) are two autoimmune disorders that have a young female preponderance, relapsing-remitting course, and positive antinuclear antibodies. The coexistence of SLE and MG has been reported in the literature with the majority of cases MG preceding SLE diagnosis1. There has been no controlled epidemiological study to prove a real association between these two diseases.
This study aims to estimate the prevalence of SLE among MG patients compared to non-MG patients and to study the demographics of the MG patients who developed SLE preceding or following MG diagnosis.
Methods: This is a retrospective observational study using the IBM Explorys database, a pooled de-identified clinical database of > 60 million unique patients in the US with patient-level data. The Explorys collects aggregated, standardized, and normalized clinical data from different electronic health records automatically updated in near real-time. International Classification of Diseases – 9 (ICD-9) diagnosis codes were used to define SLE and MG patients. For SLE patients, the ICD code was used along with at least two rheumatologist visits for patients ≥ 18 years of age. The control group included adults ≥ 18 years of age with the exclusion of MG diagnosis. We further stratified the cohorts by adding the following variables to the search tool: age, race, gender, smoking status, thymectomy, autoimmune and miscellaneous comorbidities. The index date was defined as the date of the SLE diagnosis occurring in the MG patients. A chi-square test of association was performed along with the odds ratio (OR), its standard error, and the 95% confidence interval (CI).
Results: Prevalence rates of SLE and MG among total active patients of 59,896,040 were found to match the reported rates in the literature (0.1% and 0.04% subsequently)2,3.
Of the 26,110 patients with MG, 370 had a diagnosis of SLE (1.42%) compared to 65,000 of 59,869,730 controls (0.11%). MG patients found to have increased odds of SLE compared to control group (OR 13.38, 95% CI: 2.08 to 14.84, P < 0.0001).
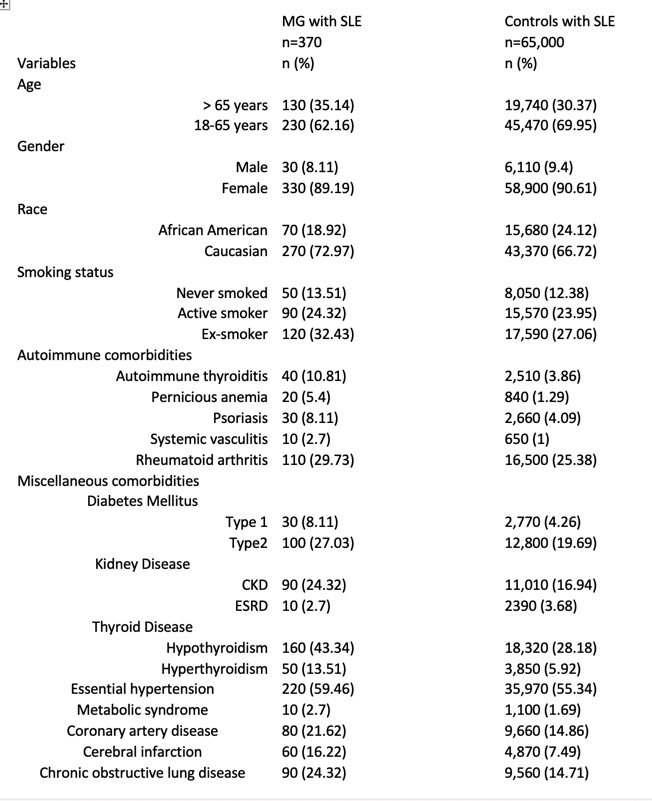
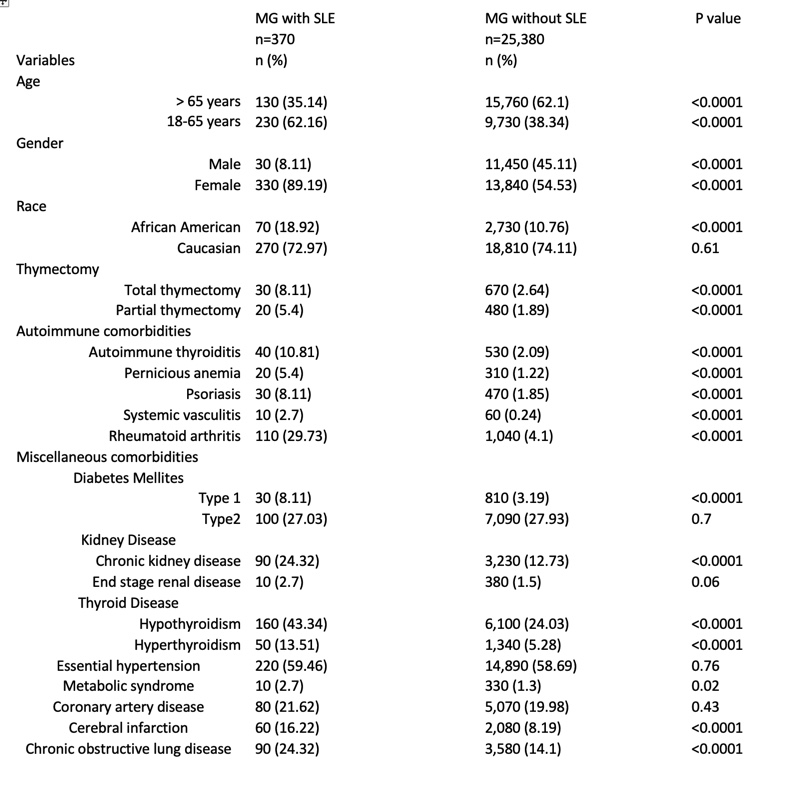
Demographics and clinical characteristics of MG patients and controls with SLE are shown in table 1. Risk factors for increased SLE risk among MG patients are shown in table 2. Female sex, African American race, thymectomy, autoimmune diseases, and miscellaneous comorbidities such as thyroid disease were significantly more common in MG patients who developed lupus.
The MG cohort who underwent thymectomy (n = 730) had an increased risk of SLE (30 out of 730) compared to MG patients who didn’t undergo thymectomy (340 out of 25,380), (OR 3.11, 95% CI: 2.12 to 4.55, P < 0.0001).
Conclusion: Our study strongly supports the higher prevalence of SLE in MG patients and highlights the risk factors of the development of lupus in MG patients. MG patients should be evaluated for the coexistence of SLE especially in post-thymectomy patients and the young African American women with a history of other autoimmune diseases. Additionally, assessment for MG is suggested in lupus patients with unexplained muscular weakness.
References:
1. Cureus (2020);12(6): e8422.
2. Rheumatology (Oxford). 2017 Nov 1;56(11):1945-1961.
3. Seminars in Neurology (2004); 24(1): 17-20
 EE985C32-EAF4_4E65-9B9C-8465839B68FE.jpeg”
EE985C32-EAF4_4E65-9B9C-8465839B68FE.jpeg”
 F018A003-73EF_44D8-8A2F_39BAD07D96BE.jpeg”
F018A003-73EF_44D8-8A2F_39BAD07D96BE.jpeg”
To cite this abstract in AMA style:
Merjanah S, Igoe A, Kaelber D, Scofield R. Association Between Systemic Lupus Erythematosus and Myasthenia Gravis: A Population-Based National Study [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/association-between-systemic-lupus-erythematosus-and-myasthenia-gravis-a-population-based-national-study/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-between-systemic-lupus-erythematosus-and-myasthenia-gravis-a-population-based-national-study/
