Session Information
Date: Wednesday, November 15, 2023
Title: Abstracts: SLE – Diagnosis, Manifestations, & Outcomes IV: Outcomes & Comorbidity
Session Type: Abstract Session
Session Time: 11:00AM-12:30PM
Background/Purpose: SLE has one of the highest 30-day hospital readmission rates among chronic conditions1. Frailty is common2 and associated with hospitalization3 in SLE, but whether frailty is associated with worse outcomes after hospital admission, including readmissions, is unknown. Our objective was to evaluate the association between frailty status and risk of readmissions, inpatient mortality at readmissions, and cost of admission among patients with SLE.
Methods: Using ICD-10 codes, we identified adults >18 years of age within the National Readmissions Database who had a primary or secondary diagnosis of SLE and were hospitalized between January and June 2018. We excluded patients who died during the index hospitalization, had an elective hospitalization, were transferred from another hospital, or were missing length of stay (LOS) or total cost values. Using the validated claims-based Hospital Frailty Risk Score4, we categorized individuals as either frail (score≥5) or non-frail (score<5) at the time of index hospitalization. Age, sex, insurance type, household income, Elixhauser Comorbidity Index (ECI), and LOS were extracted from the dataset. Primary outcome was readmission rates following discharge from the index hospitalization. Secondary outcomes included inpatient mortality, and the economic burden of hospitalizations. We compared baseline characteristics and primary and secondary outcomes between frail and non-frail patients with SLE using descriptive statistics. We used Cox proportional hazard models to estimate the association between frailty and risk of readmissions, after adjustment for relevant covariates.
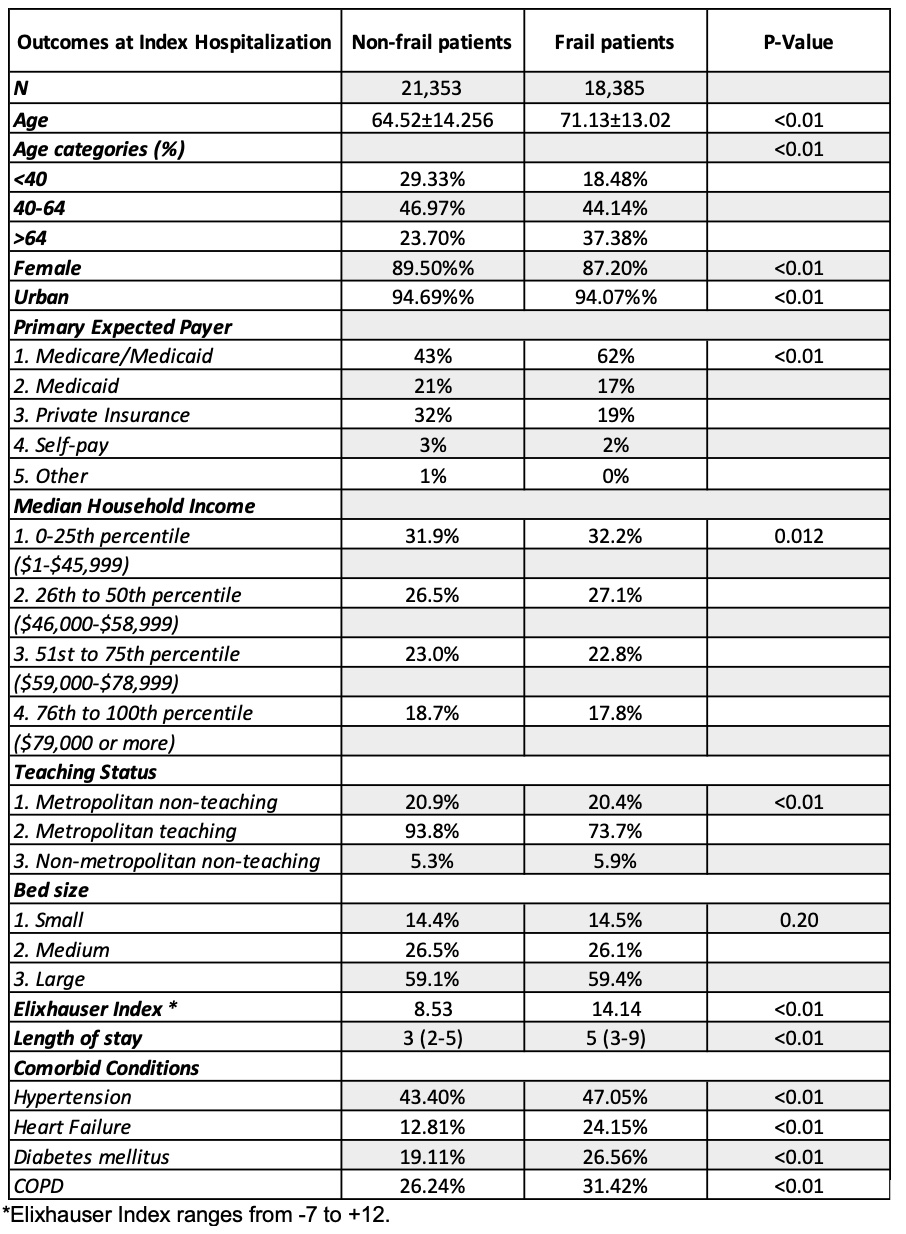
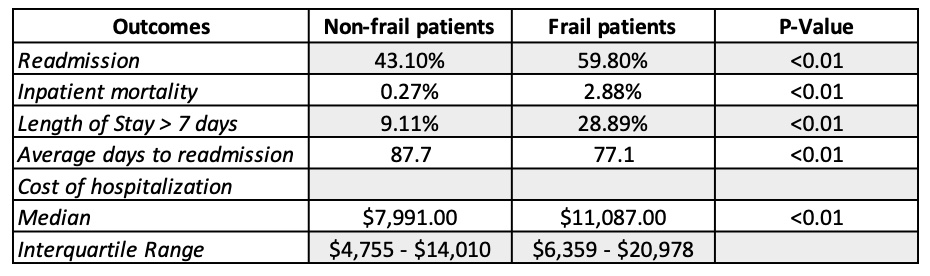
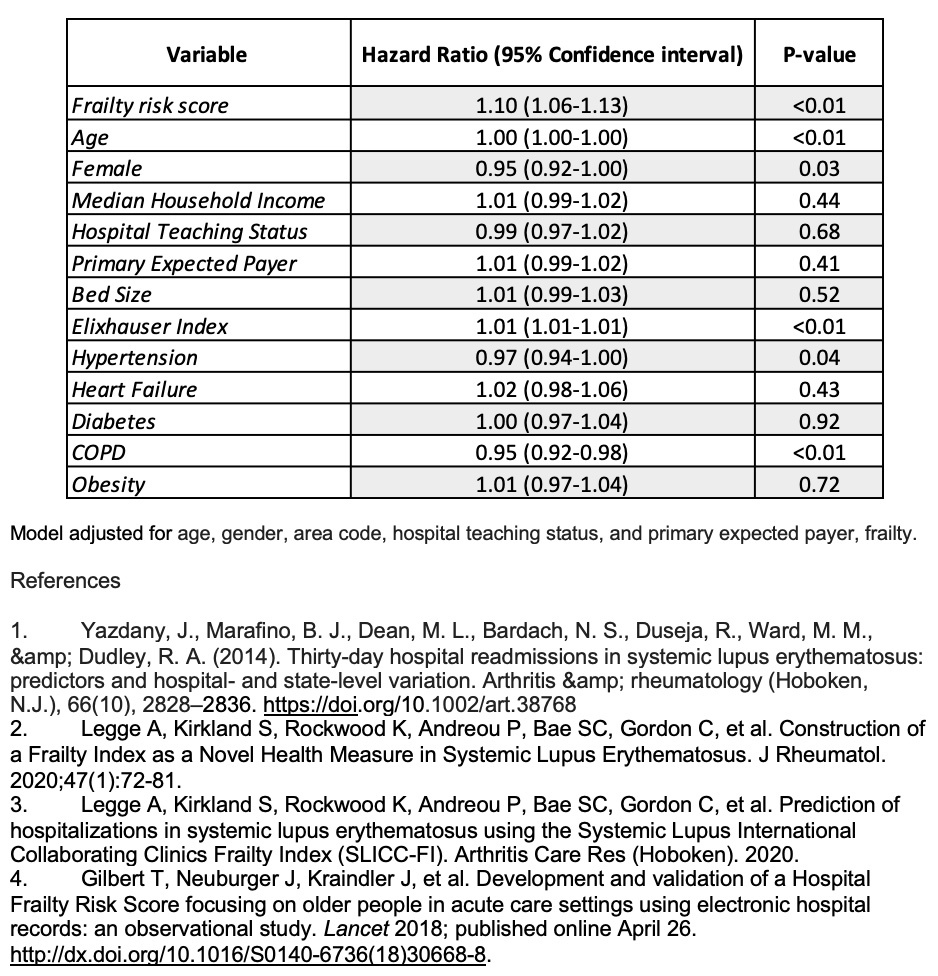
Results: We identified 39,738 patients with SLE admitted during the study period. Over a median follow-up of 9 months, frail patients with SLE (n = 18,385, 46.3%) were older with Medicare/Medicaid coverage and had higher ECI scores and longer LOS compared to non-frail patients with SLE (n = 21,353, 53.7%) (Table 1). Frail patients with SLE had more prolonged hospitalizations defined by LOS > 7 days with higher costs per hospitalization. Readmission rates in frail patients with SLE were significantly higher. At index hospitalization, frail patients had significantly higher inpatient mortality and fewer days-to-readmission on average (Table 2). In multivariable Cox proportional hazard analysis, frailty was independently associated with a 10% higher risk of readmission after adjustment for covariates (Table 3).
Conclusion: Among patients with SLE who were hospitalized, frailty is associated with more readmissions, higher mortality, and greater economic burden of hospitalization as compared to non-frail SLE patients. Assessing frailty status may help risk stratify patients with SLE at higher risk for readmission. Further research is needed to determine strategies to reduce frailty in patients with SLE in order to decrease readmission rates and other adverse health outcomes.
To cite this abstract in AMA style:
Leung C, Tahir W, Rosli Y, Lieber S, Makris U, Goulabchand R, Singh S, Singh N. Association Between Frailty and Readmissions in Hospitalized Patients with Systemic Lupus Erythematosus (SLE) [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/association-between-frailty-and-readmissions-in-hospitalized-patients-with-systemic-lupus-erythematosus-sle/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-between-frailty-and-readmissions-in-hospitalized-patients-with-systemic-lupus-erythematosus-sle/