Session Information
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose:
We investigated the association between the presence of antiphospholipid
antibodies (aPL) and/or
lupus anticoagulant (LAC) (aPL/LAC+) and all-cause
mortality among end stage renal disease (ESRD) patients with and without
SLE. We hypothesized that aPL/LAC+ would be
associated with increased cause-mortality in ESRD, with elevated risk in SLE
vs. non-SLE ESRD.
Methods: We
included patients over 18 years old with ESRD, followed at an urban tertiary
care center between 1/1/2006 and 1/31/2014 who had aPL measured at least once after initiating
hemodialysis. All SLE patients met ACR/SLICC criteria. APL/LAC+ was
defined as anti-cardiolipin IgG or IgM > 40 IU,
anti-b2glycoprotein I IgG or IgM > 40 IU,
or positive LAC.
Age, sex, race, comorbidities, anticoagulation, and potential reasons for aPL measurement were ascertained
from the medical records. Deaths through 1/31/2014 were captured in
linked National Death Index data. Time to death was defined from the first aPL measurement; otherwise,
subjects were censored at renal transplant, last visit date, or
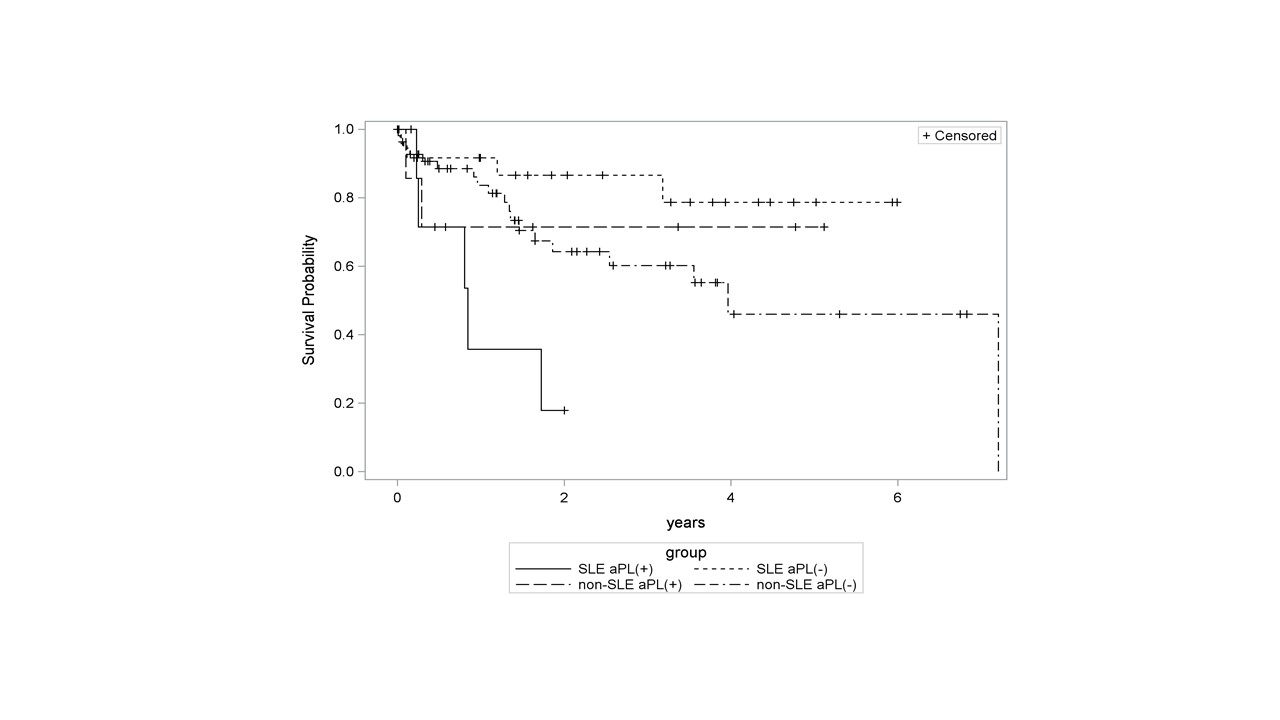
1/31/2014. Kaplan-Meier survival curves and Cox proportional hazards
model were used to evaluate the effects of aPL/LAC
and SLE status on all-cause mortality.
Results: 34 SLE ESRD
and 64 non-SLE ESRD were identified. SLE ESRD patients were younger
(40.4±12.5 vs. 51.9±18.1 years, p=0.001) and more were women (88.2% vs. 54.7%,
p=0.0007) compared to non-SLE ESRD. The frequency of aPL/LAC+
was 24% in SLE and 13% in non-SLE ESRD (p=0.16). Anticoagulation use was not
associated with SLE or mortality. Median (IQR) follow-up time was 1.6
(0.3, 3.5) years in SLE, and 1.4 (0.4, 3.2) years in non-SLE, p=0.74. In total,
30 patients died during the study period. The median (IQR) time to death was
0.3 (0.2, 0.8) years in the aPL/LAC+ group, and 1.2 (0.2, 1.9) years in the
aPL/LAC- group, p=0.22. Kaplan-Meier curves stratified by SLE and aPL/LAC
status are shown in Figure. The survival curve for SLE aPL/LAC+ group was significantly different from the SLE aPL/LAC- group (logrank
p=0.001). In Cox regression model adjusted for comorbidities, there was a
multiplicative interaction between aPL/LAC and SLE
with respect to mortality (p=0.05) indicating the differential effect of aPL/LAC+ in SLE and
non-SLE. In SLE, the adjusted hazard ratio (HR) for death for the aPL/LAC+ vs. aPL/LAC- was 9.93
(95%CI 1.33, 74.19). In non-SLE, the adjusted HR (95%CI) for aPL/LAC+ vs. aPL/LAC- was 0.77
(0.14, 4.29).
Conclusion: SLE
ESRD patients with aPL/LAC have higher risks of
all-cause mortality than do SLE ESRD patients without these antibodies and
non-SLE ESRD patients with these antibodies. Future studies will examine causes
of death. If confirmed in prospective studies, preventive strategies
could target this high risk group.
Figure 2.
Kaplan-Meier curves for the 4 groups stratified by SLE and aPL status.
To cite this abstract in AMA style:
Broder AR, Mowrey W, Kim M, Murakhovskaya I, Neugarten J, Costenbader KH, Putterman C. Association Between Antiphospholipid Antibodies and All-Cause Mortality Among End Stage Renal Disease Patients with and without SLE [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/association-between-antiphospholipid-antibodies-and-all-cause-mortality-among-end-stage-renal-disease-patients-with-and-without-sle/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-between-antiphospholipid-antibodies-and-all-cause-mortality-among-end-stage-renal-disease-patients-with-and-without-sle/