Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
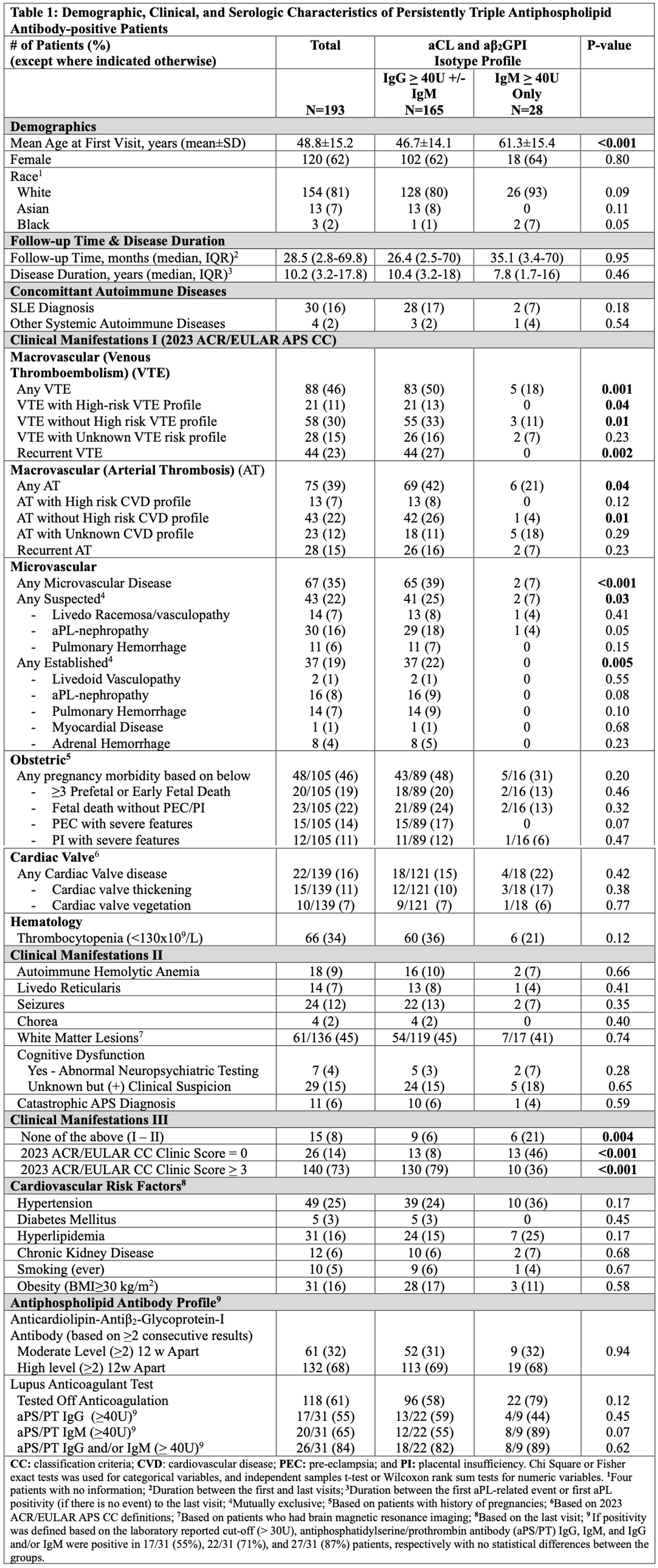
Background/Purpose: Triple aPL-positive (lupus anticoagulant test [LA], anticardiolipin antibody (aCL), and anti-β2 glycoprotein-I antibody [aβ2GPI]) patients are at higher risk to develop a severe clinical phenotype, compared to double or single aPL-positive patients. Our primary objective was to evaluate the characteristics of triple aPL-positive patients based on 2023 ACR/EULAR Antiphospholipid Syndrome (APS) Classification Criteria (CC) clinical and laboratory domains. Secondly, we compared triple aPL-positive patients with different aCL/aβ2GPI isotypes.
Methods: For this retrospective analysis of an APS-specialized practice cohort, after identifying patients via electronic medical records who were evaluated for “aPL-positivity” (Feb 2016 to May 2024), we analyzed the demographic, clinical (including ACR/EULAR APS CC Clinical Domains), and serologic characteristics of triple aPL-positive patients (defined as persistently positive LA test, aCL IgG/M ≥ 40 ELISA Units, and aβ2GPI IgG/M ≥ 40 ELISA Units). For the secondary analysis, we compared the characteristics of triple aPL-positive patients with different aCL/aβ2GPI isotypes, i.e., IgG (±IgM) versus IgM only.
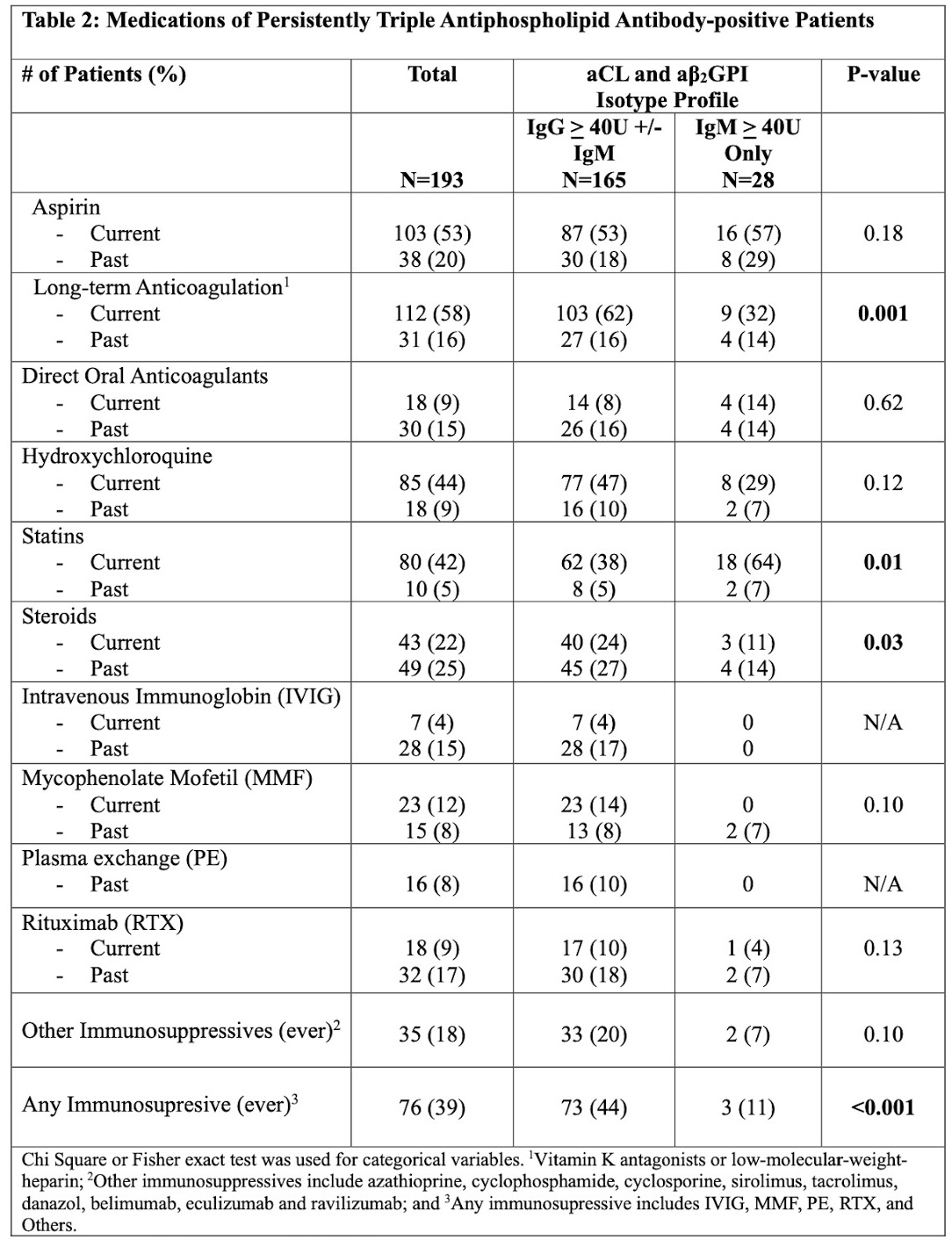
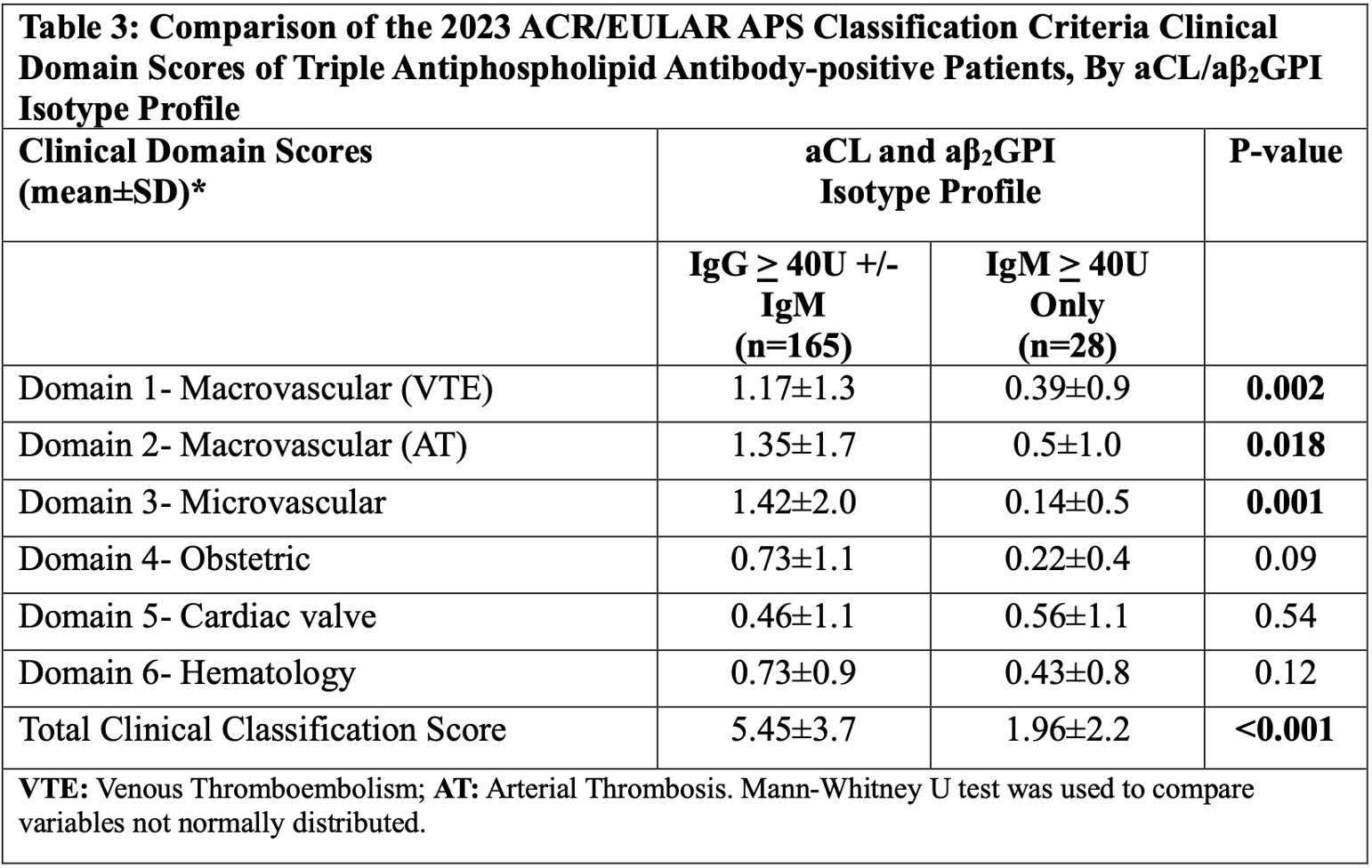
Results: Of 751 patients evaluated, 205 (27%) had triple aPL positivity; four were excluded due to non-persistent aPL and eight due to low aCL/aβ2GPI titers (20-39 U). Of the remaining 193 patients, 165 (85%) had triple aPL-positivity with aCL/aβ2GPI IgG (±IgM) and 28 (15%) IgM only (Tables 1 and 2). Based on the analysis of the entire cohort (n:193), 88 (46%) patients had macrovascular venous thromboembolism (VTE), 75 (39%) macrovascular arterial thrombosis (AT), 67 (35%) microvascular, 48 (46%) obstetric, 22 (16%) cardiac valve, and 66 (34%) hematologic domains involved. Based on the comparison of isotype profiles: a) macrovascular VTE/AT and microvascular domain involvement as well as long-term anticoagulation, steroid, and immunosuppression use were significantly more common in triple aPL-positive patients with IgG (±IgM), compared to those with IgM only, and other clinical criteria and non-criteria items were similar except a trend for preeclampsia in patients with IgG (±IgM) (p=0.07); b) almost half of patients with aCL/aβ2GPI IgM only, who were significantly older, had no ACR/EULAR APS CC clinical domain involvement ; and c) the mean ACR/EULAR APS CC clinical domain scores (total, macrovascular, and microvascular) were significantly higher in patients with aCL/aβ2GPI IgG (±IgM) (Table 3).
Conclusion: In our triple aPL-positive cohort, identified based on ACR/EULAR APS CC laboratory domains, and assessed based on clinical domains, 46%, 39%, 35%, 46%, 16%, and 34% had macrovascular VTE, macrovascular AT, microvascular, obstetric, cardiac valve, and hematology domain involvement, respectively. Given that only 15% of triple aPL-positive patients had aCL/aβ2GPI IgM isotype only, with lower ACR/EULAR APS CC clinical domain scores compared to those with aCL/aβ2GPI IgG (±IgM), our findings support the need for both mechanistic and clinical studies investigating the pathogenic and diagnostic role of aCL/aβ2GPI IgM isotype, even in the presence of LA-positivity.
To cite this abstract in AMA style:
Kose Cobanoglu R, Vega J, Burgos C, Erkan D. Assessment of Triple Antiphospholipid Antibody-positive Patients Based on Clinical and Laboratory Domains of 2023 ACR/EULAR Antiphospholipid Syndrome Classification Criteria [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/assessment-of-triple-antiphospholipid-antibody-positive-patients-based-on-clinical-and-laboratory-domains-of-2023-acr-eular-antiphospholipid-syndrome-classification-criteria/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/assessment-of-triple-antiphospholipid-antibody-positive-patients-based-on-clinical-and-laboratory-domains-of-2023-acr-eular-antiphospholipid-syndrome-classification-criteria/