Session Information
Date: Monday, November 8, 2021
Title: Osteoporosis & Metabolic Bone Disease – Basic & Clinical Science Poster (1135–1149)
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: The twenty first century has seen falling reimbursement rates for dual energy X-ray absorptiometry (DXA) testing coupled with a rising elderly population in the U.S. The purpose of this study was to assess trends in performing DXA scans among U.S. medical providers and the resulting potential impact of reduced DXA availability on access to care.
Methods: A retrospective review was performed on publicly available data Medicare provider utilization and payment data between 2012 and 2018. Data was accessed from the CMS website and filtered for CPT codes used for reimbursement of DXA testing. This data included information on provider (name and identifier), city, state, zip code, sex, procedure type, location (office-based providers vs hospital-based providers), and provider specialty. Provider zip codes were compared to the Federal Office of Rural Health Policy (FORHP) designation as rural areas.
Results: From 2012-2018 the standardized number of DXA tests per 100,000 women decreased from 5,641 to 4,899 DXA tests per 100,000 women with a nadir of 4,307 DXA tests per 100,000 women in 2015. The number of DXA providers reimbursed located in a rural zip code decreased 41.3% (from 2,945 to 1,728), similar to the relative decrease in the proportion of rural providers (from 14.2% to 9.0%). The percentage of reimbursed DXA scans performed by rheumatologists decreased from 10.3% to 7.1%, internal medicine from 22.0% to 12.7%, obstetrics/gynecology from 6.5% to 4.2%, and family practice from 11.3% to 8.0%; diagnostic radiology, which are hospital-based providers, increased from 31.6% to 50.4% during the same time period.
Conclusion: The standardized number of DXA tests per 100,000 women Medicare enrollees decreased between 2012 and 2018. During the same time period, the claims for DXA testing for office-based specialties decreased, while the claims for DXA testing performed by diagnostic radiology increased. Both the number and proportion of both rural and primary care providers submitting claims for DXA testing have decreased, leading to likely decreased access to osteoporosis care among rural residents. With a progressive aging of the population, the access to tools for prevention and treatment of osteoporosis, such as DXA, is key to delivering high-quality osteoporosis care and effectively screening high risk patients.
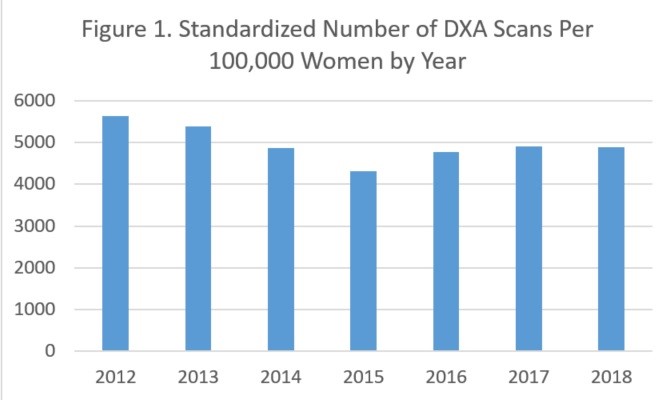 Figure 1. Standardized Number of DXA Scans Per 100,000 Women by Year.
Figure 1. Standardized Number of DXA Scans Per 100,000 Women by Year.
 Figure 2. Yearly Trends in Percentages of DXA Testing by Specialty and Year.
Figure 2. Yearly Trends in Percentages of DXA Testing by Specialty and Year.
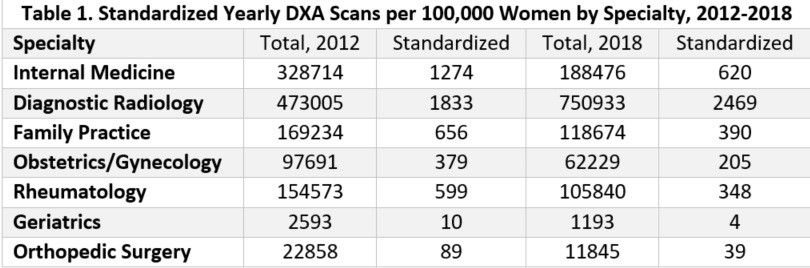 Table 1. Standardized Yearly DXA Scans Per 100,000 Women by Specialty, 2012_2018. Columns sorted by: Total number of DXA scans in 2012; Number of DXA scans standardized per 100,000 women in 2012; Total number of DXA scans in 2018; Number of DXA scans standardized per 100,000 women in 2018.
Table 1. Standardized Yearly DXA Scans Per 100,000 Women by Specialty, 2012_2018. Columns sorted by: Total number of DXA scans in 2012; Number of DXA scans standardized per 100,000 women in 2012; Total number of DXA scans in 2018; Number of DXA scans standardized per 100,000 women in 2018.
To cite this abstract in AMA style:
Edgil T, Saag K, Curtis J, Danila M. Assessing Trends in Dual Energy X-Ray Absorptiometry (DXA) Utilization Among Medical Providers in the United States [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/assessing-trends-in-dual-energy-x-ray-absorptiometry-dxa-utilization-among-medical-providers-in-the-united-states/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/assessing-trends-in-dual-energy-x-ray-absorptiometry-dxa-utilization-among-medical-providers-in-the-united-states/
