Session Information
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Opioids are often prescribed for osteoarthritis (OA) pain management despite the need for balancing their risks and benefits. Since there are no standard criteria for defining inappropriate pain management (IPM), this study examined prevalence of potential criteria that may be indicative of IPM in OA patients (pts) treated with opioids.
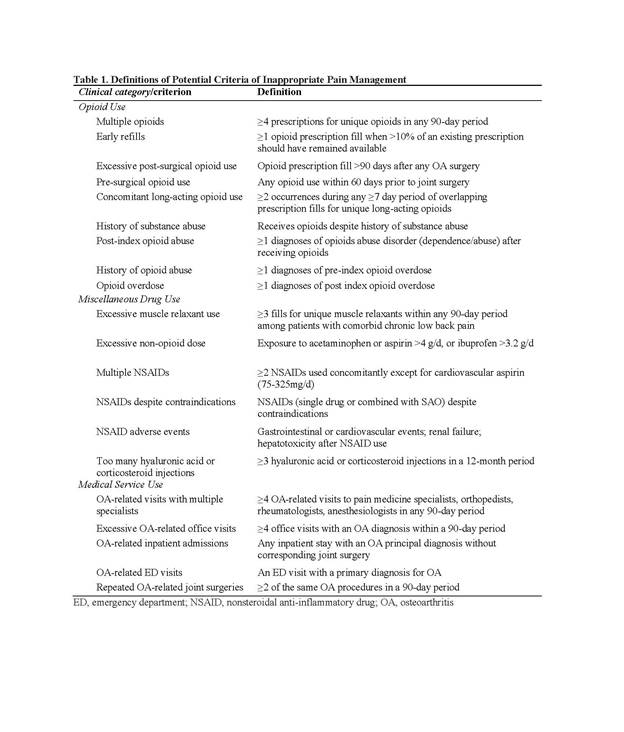
Methods: Data were from a US employer-sponsored insurance claims database (2011-2016). Pts were community-dwelling adults (≥18 yr) diagnosed with hip/knee OA who filled an opioid prescription (index event) within 30 days of OA diagnosis; had continuous enrollment 6 months pre- and 12 months post-index; and no pre-index joint surgery. Opioid regimen intensity in the 3-month post-index period was defined by frequency (intermittent: ≤4 d/wk; daily: >4 d/wk), average daily dose in morphine milligram equivalents (MME: <50 MME/d=low, ≥50 MME/d=high), and short- or long-acting opioids (SAO, LAO), providing 6 increasing intensity regimens: intermittent-low-dose SAO, intermittent-high-dose SAO, daily-low-dose SAO, daily-high-dose SAO, LAO, and LAO+SAO. Potential IPM, defined based on existing literature and clinical input (Table 1), comprised 3 clinical categories (Opioid Use, Miscellaneous Drug Use, Medical Service Use). Descriptive analysis characterized prevalence of potential IPM over the 12-month post-index period.
Results: The study included 271,512 pts (61.5% knee; 11.1% hip; 27.4% both); mean age 59.8 yr; 62.7% women. IPM was observed in 52.6% of pts during the post-index period; 30.7% in Miscellaneous Drug Use, 27.7% in Opioid Use, and 14.4% in Medical Service Use. LAO+SAO had the highest IPM (85.4%); intermittent SAO regimens had the lowest (42.7%-44.7%; Table 2). IPM in the intermittent dose regimens was driven by Miscellaneous Drug Use; IPM in the higher intensity regimens was driven by Opioid Use. The top 2 IPM criteria in each clinical category were generally similar across opioid intensity regimens (Table 2).
Conclusion: This study suggests potential criteria indicative of IPM were observed in the majority of OA pts treated with opioids. IPM generally increased with higher opioid intensity regimens; drivers of IPM differed between low and high intensity regimens. The study was limited by the data source and retrospective design such that it could not be determined if IPM resulted from the index opioid treatment regimen itself, patient/physician behavior, or other factors. Nevertheless, study findings reinforce physician need for evaluating pain management with opioids in OA pts individually to ensure optimal health outcomes.
To cite this abstract in AMA style:
Katz NP, Gandhi K, Wei W, Huang A, Wang L. Assessing Inappropriate Pain Management in Adults with Hip or Knee Osteoarthritis Treated with Different Opioid Intensity Regimens: Results from a Retrospective Database Analysis [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/assessing-inappropriate-pain-management-in-adults-with-hip-or-knee-osteoarthritis-treated-with-different-opioid-intensity-regimens-results-from-a-retrospective-database-analysis/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/assessing-inappropriate-pain-management-in-adults-with-hip-or-knee-osteoarthritis-treated-with-different-opioid-intensity-regimens-results-from-a-retrospective-database-analysis/