Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: There is high-quality evidence that prompt diagnosis and treatment have beneficial impact on outcomes in RA. Current guidelines from both North America and Europe reflect this evidence base. Despite this, there is marked variation in how clinicians follow guidance. We conducted a national survey of practice in England and Wales to assess adherence to guidelines focussing on time to first disease modifying treatment. We have already published from this, demonstrating that over a third of patients experience significant delays. Accepting that data collected outside of a clinical trial or research environment tend to be less complete, we hypothesized that the completeness of data returned would be directly correlated with the quality of care provided.
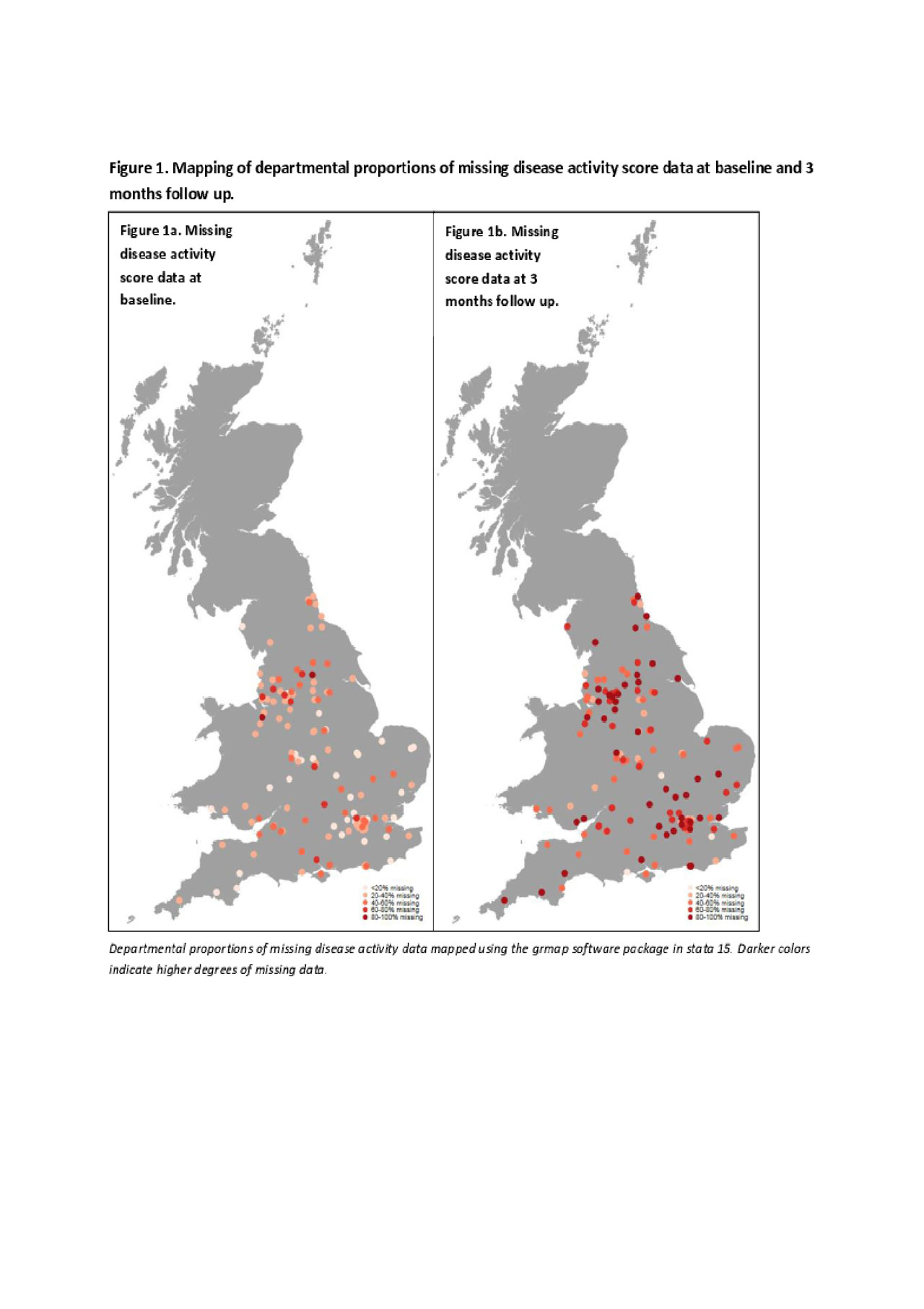
Methods: Data were collected between January 2014 and December 2015 on patients referred to specialist rheumatology services across England and Wales with a suspected diagnosis of inflammatory arthritis. Baseline demographic and clinical details, including a disease activity score (DAS-28), were collected. Patients with a confirmed diagnosis of RA had follow up data collected at three months. Demographic differences in patients with missing DAS-28 data at baseline or three months follow up were tabulated. Departmental proportions of missing DAS-28 data across England and Wales were mapped. A mixed effects logistic regression model adjusted for patient and department level variables was conducted to assess if completeness of baseline DAS-28 data associated with prompt disease modifying treatment commencement.
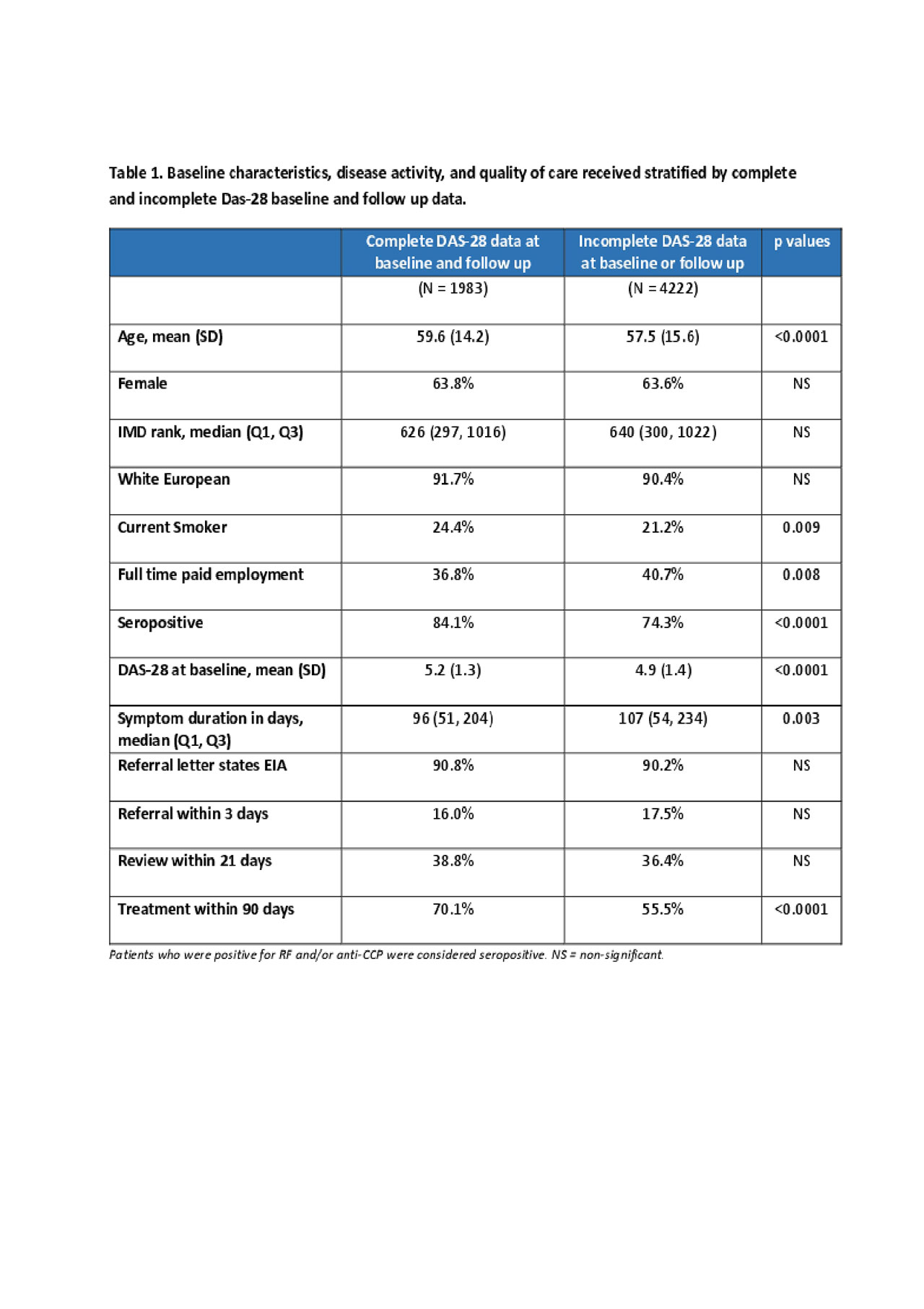
Results: 6,205 patients diagnosed with RA from 136 rheumatology departments had data, of whom 3,733 (60%) commenced a DMARD within 3 months of referral to specialist rheum care. Disease activity data (measured using DAS-28) was available for 4,075 (66%) at baseline and 2,341 (38%). Patients with missing DAS-28 data had distinct characteristics to those with complete data, see table 1.
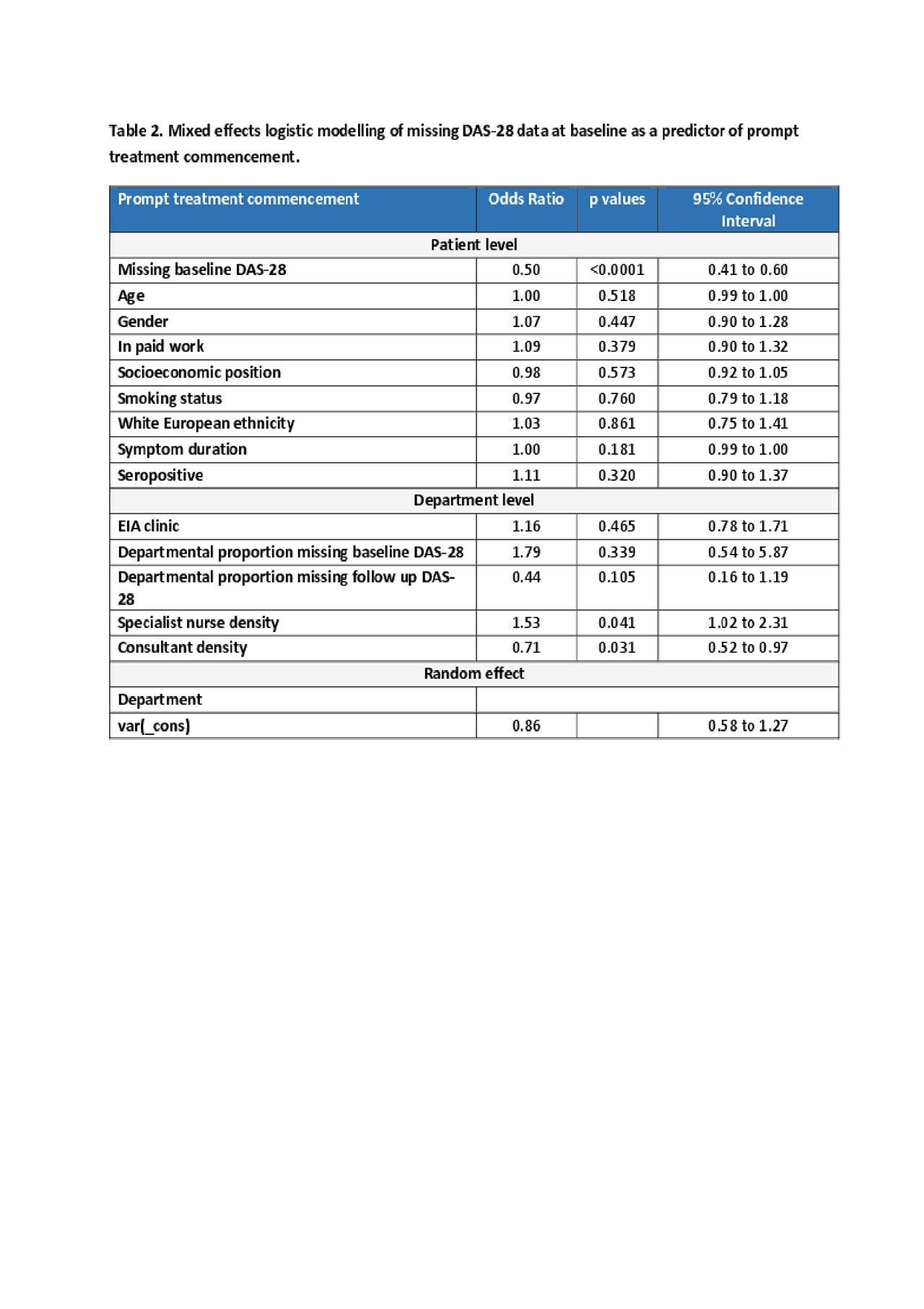
Patients without a baseline DAS-28 score recorded were 50% less likely (odds ratio 0.50, 95%CI 0.41 to 0.60) to commence a DMARD within three months. This effect was independent of all patient level factors included in the analysis. Unit level factors including staff ratios did correspond to data quality, and in particular greater specialist nurse support correlated with higher quality care. See table 2 for further details.
There were broad geographic variations in departmental proportions of missing data, illustrated in figure 1. The departmental proportion of missing DAS-28 data ranged from 0 to 91% at baseline, and 0.1 to 100% at 3 months follow up.
Conclusion: These data from a large national survey demonstrate a clear relationship between the completeness of data collected and the quality of care provided. This supports the view that clinician engagement in quality assessment is likely to be a good surrogate for the quality of care that they are delivering. Measuring quality in healthcare has climbed up the rheumatology community’s agenda in the last decade, reflected in the ACR white paper on performance outcome measure in 2016. Data completeness is a simple but useful additional metric as a surrogate for quality.
To cite this abstract in AMA style:
Yates M, Norton S, MacGregor A, Bechman K, Rampes S, Galloway J. Assessing Care Quality in Rheumatology Services [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/assessing-care-quality-in-rheumatology-services/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/assessing-care-quality-in-rheumatology-services/