Session Information
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Tuberculosis (TB) infection is an important cause of morbidity and mortality in systemic lupus erythematosus (SLE) patients, especially in developing countries. Previous studies have shown that higher cumulative doses of glucocorticoids within the last year are a risk factor for Mycobacterium tuberculosis infection. However, the role of conventional immunosuppressants in TB development is controversial. The aim of this study was to identify the factors associated with TB infection in SLE patients.
Methods: A retrospective case-control study. From January 2007 to December 2017, a total of 268 patients who met the 1997 ACR revised classification criteria for SLE were included. Cases were SLE patients diagnosed with TB by clinical, radiological, microbiological, molecular and/or histopathological criteria (SLE-TB). TB infection was classified as pulmonary, extrapulmonary or disseminated. Controls were SLE patients without TB infection (SLE-non-TB). In total 67 cases and 201 controls were assessed. The quantitative variables are expressed as means or medians with their respective measure of dispersion and the qualitative variables as absolute number and percentage. Univariable and multivariable logistic regression analyses were performed.
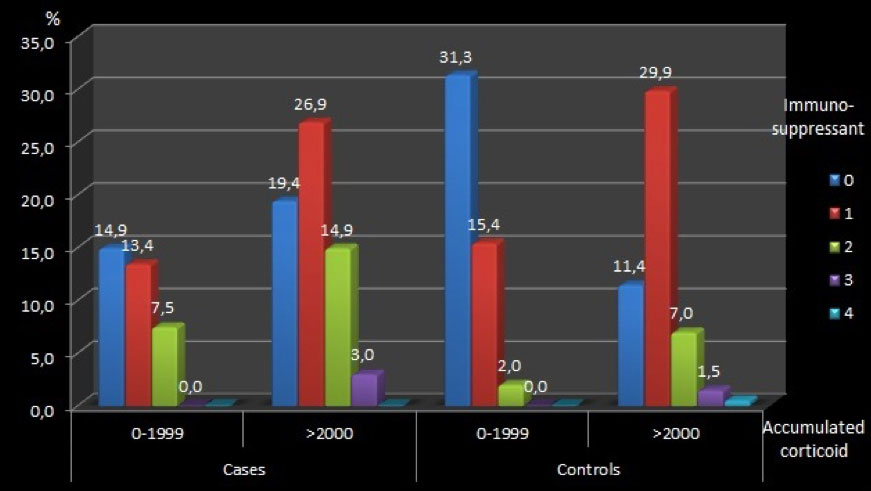
Results: Females were more frequent in cases (83.5%) and controls (86%). The mean age was 34 years (range 13-84 years) for cases and 36 years (range 10-87 years) for controls. No significant differences in the frequency of comorbidities [diabetes, cirrhosis and Charlson comorbidity index (CCI)], disease duration and disease activity (SLEDAI) between cases and controls were found. Pulmonary TB occurred in 46.3%, extrapulmonary TB in 16.4% and disseminated TB in 37.3% of cases. Miliary pattern on chest X-ray was found in 23.8% of cases. In the univariable analyses, kidney transplantation, cumulative glucocorticoid dose ( >2 grams) and ≥2 immunosuppressants received within the last year were associated with TB infection (11.9% in cases vs. 4.4% in controls; p= 0.04; 3.7 grams in cases vs. 2.1 grams in controls, p = 0.02; 22.7% in cases and 8.9% in controls, p= 0.02, respectively) (figure 1). By multivariable analysis, after adjusting for age, gender, disease duration, nephritis, antimalarials, immunosuppressants and CCI, cumulative glucocorticoid dose (OR 1.00; 95% CI 1.00-1.01; p=0.02) and kidney transplantation (OR 4.1; 95% CI 1.06-16.1; p=0.04) were significantly associated with TB infection occurrence. The most commonly immunosuppressants used were mycophenolate mofetil (MMF), azathioprine and cyclophosphamide, with a higher prevalence of MMF and rituximab in SLE-TB compared with SLE-non-TB patients (35.8% vs. 22.9% and 9% vs. 3%, respectively) (Figure 2).
Conclusion: Besides cumulative glucocorticoid dose ( >2 grams), kidney transplantation was found to be significantly associated with an increased risk of Mycobacterium tuberculosis infection. Although, the exposure to ≥2 immunosuppressants was more than twice in cases than in controls, it was not significant in multivariable analysis. Prospective studies are needed to clarify the potential risk of immunosuppressants for TB infection development in SLE.
To cite this abstract in AMA style:
Coral-Enriquez J, Restrepo M, Vasquez G, Muñoz-Vahos C, Jaramillo D, Vanegas-García A, Eraso R, Hernández J, Jaimes F, Gonzalez L. Are Immunosuppressants a Risk Factor Associated with Mycobacterium Tuberculosis Infection in Colombian Patients with Systemic Lupus Erythematosus? A Case-control Study [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/are-immunosuppressants-a-risk-factor-associated-with-mycobacterium-tuberculosis-infection-in-colombian-patients-with-systemic-lupus-erythematosus-a-case-control-study/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/are-immunosuppressants-a-risk-factor-associated-with-mycobacterium-tuberculosis-infection-in-colombian-patients-with-systemic-lupus-erythematosus-a-case-control-study/