Session Information
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: Familial Mediterranean fever (FMF) is a monogenic autoinflammatory disease that is characterized by recurrent episodes of polyserositis. Episodes typically consist of fever, peritonitis, and arthritis. This peritonitis of the FMF is frequently misdiagnosed as acute abdomen. Acute appendicitis is the leading cause of acute abdomen thus surgical interventions are not uncommon in the case of FMF peritonitis. In this study, we analyzed FMF patients with appendectomies to determine whether FMF patients are still misdiagnosed as appendicitis.
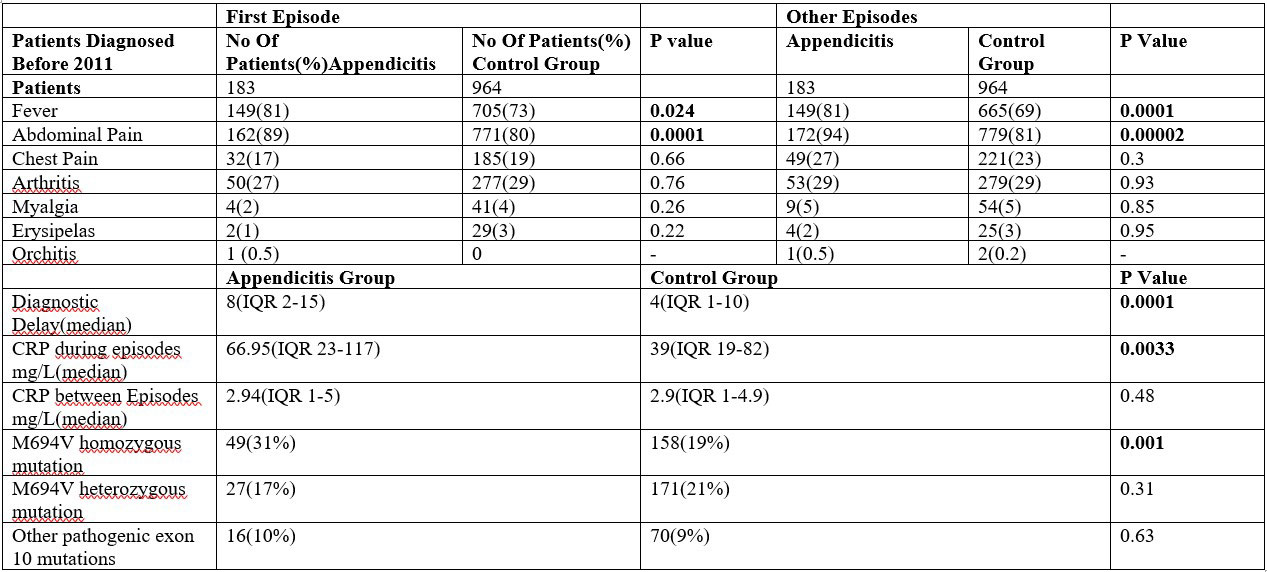
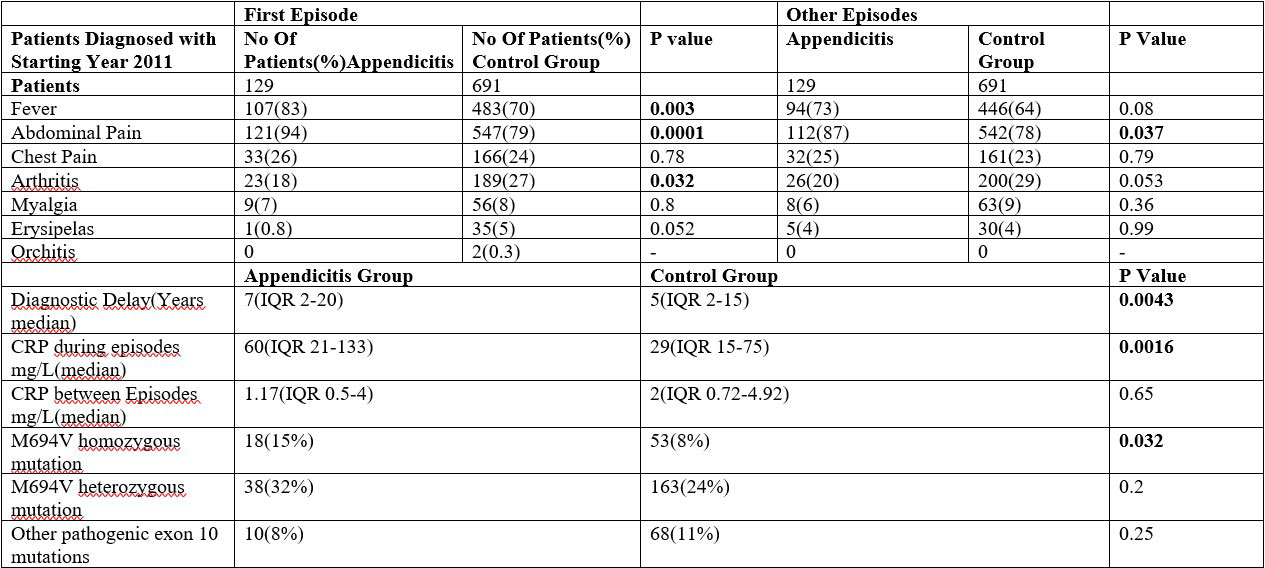
Methods: We reviewed 303 FMF patients with unindicated appendectomies and matched 1655 FMF patients without unindicated appendectomies for comparison. We classified patients according to the year at the time of the diagnosis [Series 1(diagnosis before 2011) and Series 2(diagnosis starting with 2011)]. We analyzed clinical manifestations, genetic mutations, diagnostic delay, and acute phase reactant levels.
Results: 183 patients in the appendectomy group and 964 patients in the control group classify within the series 1. 120 patients in the appendectomy group and 691 patients in the control group classify within the series 2. For series 1 and 2 in the first episode in the appendectomy group fever and abdominal pain were more common and statistically significant in both. Arthritis, myalgia, and erysipelas were more common in the control group but none of these findings were statically significant in both groups. Chest pain was similar in both appendectomy and control groups. In the following episodes for series 1 and 2 the results were the same except fever was being more common for series 2 while being statically insignificant [Table1, Table2]. Diagnostic delays were longer for the appendectomy group [median 8vs4 years (series1), 7vs5 years (series2)]. CRP levels during episodes were higher for appendectomy group [median 66.95vs39 mg/L (series1), 60 vs 29 mg/L(series2)]. CRP levels between episodes are inconclusive. Pathogenic exon 10 mutations were more common for the appendectomy group overall in both series. M694V homozygous mutations were more common within the appendectomy group (both series) and statistically significant. Other mutations were statistically insignificant [Table1, Table2]. Appendectomy rates between series were not significant [18.98%vs18.66%, p: 0.94).
Conclusion: At this age, even 25 years after the identification of the MEFV gene diagnosis of FMF is still challenging and late diagnosis is not uncommon. Our study revealed appendectomy rates before FMF at 15.8% and the appendectomy group has a significantly longer diagnostic delay. M694V homozygous mutations were associated with appendicitis misdiagnosis and severity of the disease. CRP levels were higher in the appendectomy group revealing more severe episodes although this biomarker is ineffective for differing FMF from appendicitis. In the light of this knowledge, a new biomarker is required for FMF diagnosis in the case of acute abdomen.
To cite this abstract in AMA style:
Başpınar Ş, Alkan A, Yuzbasioglu M, Yenigun S, Ayla A, Durucan I, Candan M, Karabiçek A, Belli Ç, Bayraktar T, Besiroglu H, Ozdogan H, Ugurlu S. Appendicitis Still a Challenge for FMF Patients? [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/appendicitis-still-a-challenge-for-fmf-patients/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/appendicitis-still-a-challenge-for-fmf-patients/