Background/Purpose: Antiphospholipid-associated nephropathy (APLN) is characterized by coexistence of antiphospholipid antibodies (aPLs) and renal small-vessel vasculopathy/chronic renal ischemia. Consequences of APLN to thrombosis have yet to be known. We aimed in this study to clarify the characteristics and thrombotic risk of APLN in patients with lupus nephritis (LN).
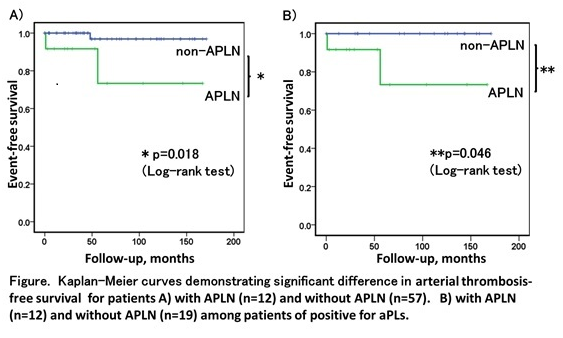
Methods: Patients with LN proven by renal biopsy from January 2000 to February 2014 were included. A total of 90 patients were histologically diagnosed as having LN according to the ISN/RPS classification. APLN was diagnosed when both aPLs and at least one of the following pathological features were present, thrombotic microangiopathy (TMA), fibrous intimal hyperplasia (FIH), fibrocellular arterial occlusion (FAO), focal cortical atrophy (FCA) or tubular thyroidization (TUB) according to the criteria (Miyakis S et al. J Thromb Haemost 2006). Patients with antiphospholipid syndrome were excluded. aPLs including lupus anticoagulant, IgG/M anticardiolipin antibody, IgG/M anti-b2-glycoprotein I antibody and IgG/M phosphatidylserine dependent antiprothrombin antibody were measured. Clinical features of APLN patients were retrospectively analyzed. Development of arterial thrombosis was retrospectively observed. Log-rank test was introduced for the comparison between those with APLN and without.
Results: Among 90 patients with biopsy-proven LN, 21 were excluded (10 with APS, 5 without tests for aPLs and 6 for other reasons) and the rest 69 patients were recruited in the study. The median age and mean disease duration was 33 years old and 4.8 years, respectively. Twelve patients (17.4%) were diagnosed as APLN (9 FCA, 5 FIH, 1 FAO and 1 TUB) and 10 as APLN-like disease without aPL and with pathological features. Patients with APLN had higher frequency of hypertension (p-value by chi-square test =0.002). APLN patients more frequently developed arterial thrombosis during the median observation period of 53 months (p-value by log-rank test = 0.018) compared with patients without APLN. Among patients positive for aPLs,
Conclusion: APLN was found in 17% of LN and associated with hypertension. APLN with LN is a possible risk for developing arterial thrombosis, although prospective study in a larger cohort would be necessary.
Disclosure:
T. Fukui,
None;
S. Yasuda,
None;
T. Watanabe,
None;
K. Ohmura,
None;
S. Shimamura,
None;
I. Nakagawa,
None;
A. Noguchi,
None;
H. Shida,
None;
Y. Shimizu,
None;
M. Kono,
None;
T. Kurita,
None;
K. Oku,
None;
T. Bohgaki,
None;
O. Amengual,
None;
T. Horita,
None;
T. Atsumi,
None.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/antiphospholipid-associated-nephropathy-is-a-risk-for-developing-arterial-thromboses-in-patients-with-systemic-lupus-erythematosus/