Session Information
Session Type: Abstract Session
Session Time: 10:00AM-10:50AM
Background/Purpose: Anticytokine biological disease modifying anti-rheumatic drugs (bDMARD), which are widely prescribed for Inflammatory Rheumatological Diseases (IRD) are currently undergoing clinical trials for the treatment of Covid-19. Despite indicators that bDMARDs ought to reduce adverse outcomes through inhibition of hyperinflammatory cytokine storm events, only one global registry of 600 Covid-19 IRD patients has indicated that pre-treatment with the tumour necrosis factor inhibitor class of bDMARD protects against hospitalisation. Furthermore global registry reports of admission rates of 46% in IRD are at variance with lower rates recently published in the NEJM, suggesting a potential reporting bias in registry data towards hospitalised patients, including those who may only become infected during hospitalisation for an unrelated condition.
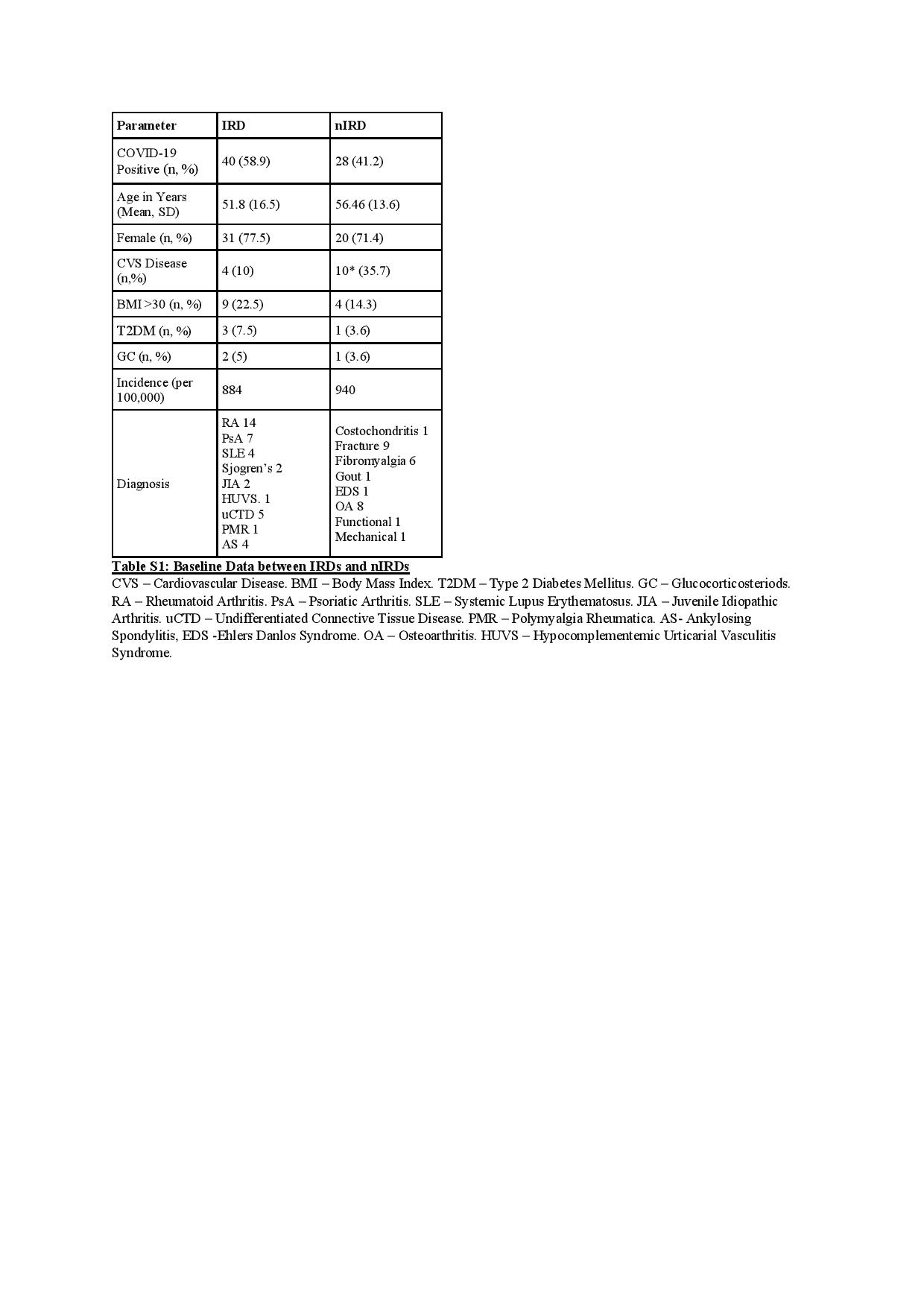
Methods: To eliminate reporting bias we contacted 7,500 patients comprising 4,524 with IRDs and 2,976 with non-inflammatory disease (nIRDs) attending Trinity College Dublin aligned academic Rheumatology centres, collecting data up to the end of the 1st pandemic wave in Ireland on 03rd June 2020. Cross-referencing with test-centre positive polymerase chain reaction (PCR) results and mortality data was performed to ensure complete collation of cases.
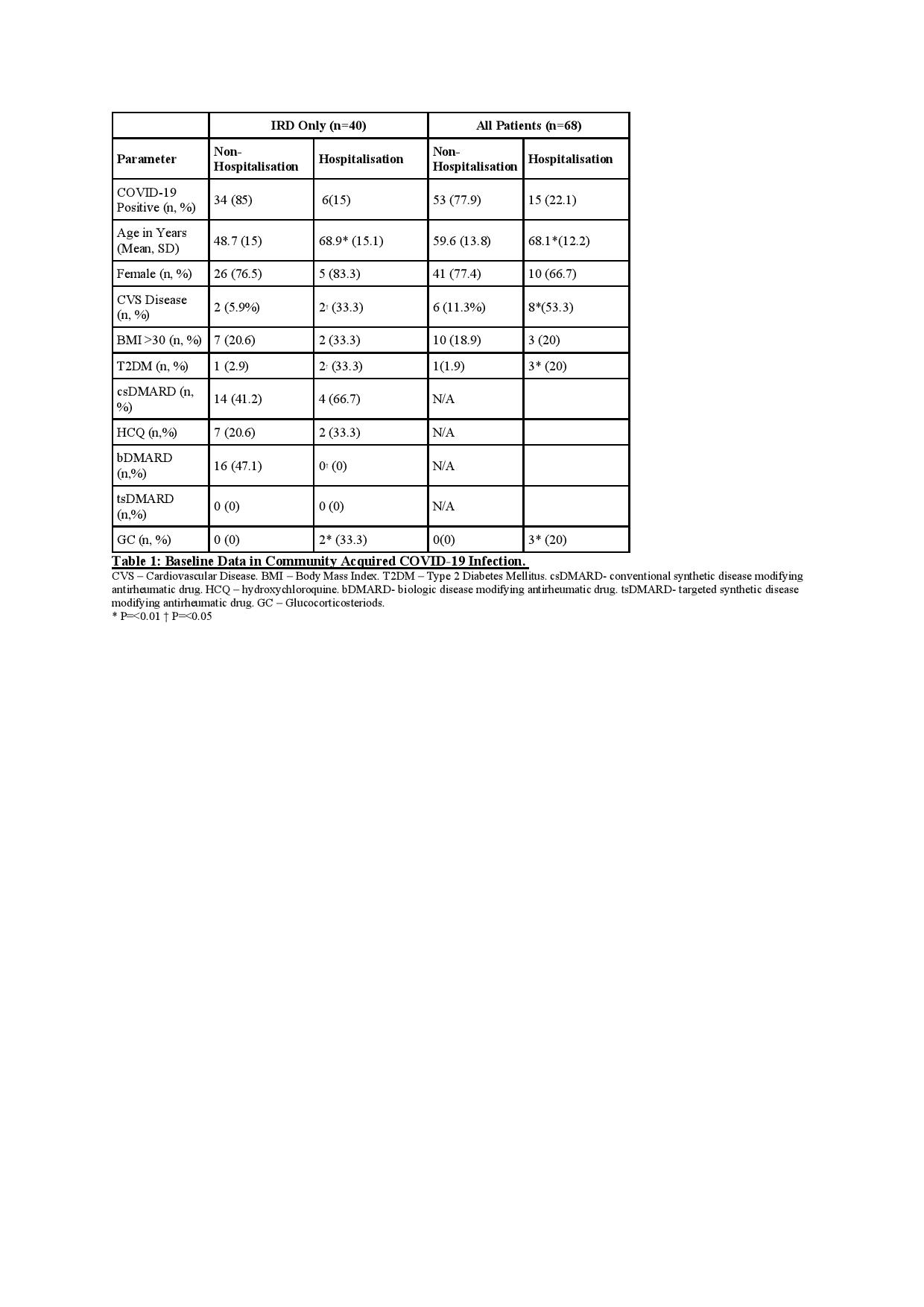
Results: We identified 77 cases of PCR or physician diagnosed COVID-19, of whom 68 were community acquired (supplementary table 1) and 9 were hospital acquired. No differences were seen in cumulative incidence/100,000 of COVID-19 between IRD (884), non-inflammatory rheumatic disorders (nIRD, 940), or incidence rates for metropolitan Dublin (887). In subgroup analysis of community acquired infection, hospitalisation was statistically less likely in patients receiving long-term anticytokine biological therapies (P< 0.05). This significance was lost when hospital acquired cases were included. In further analysis of the 40 IRD and 28 nIRD community acquired cases, hospitalisation was more likely to occur in those receiving glucocorticosteroids (p< 0.01) or those diagnosed with type 2 diabetes (p< 0.05). Lower hospitalisation rates for community acquired Covid-19 in IRD (15%), equivalent to national figures (13%) were observed.
Conclusion: Unintentional bias in reporting hospitalised COVID-19 cases to IRD registries and the inclusion of hospital acquired cases during data analysis, may lead to spurious overestimates of overall morbidity while masking critically important information on the role of anticytokine therapies in preventing hospitalisation. Although our dataset is small, these results suggest a much more powerful role for anticytokine therapies in treating COVID-19 than existing published registry data indicate. Further analysis using existing datasets on community acquired cases, are likely to more rapidly identify existing drugs to treat COVID-19, which are urgently required to improve health outcomes.
To cite this abstract in AMA style:
Flood R, Conway R, Kane D, Mullan R. Anticytokine Therapies for Inflammatory Rheumatic Disease (IRD) Are Associated with Reduced Hospitalisation Following Community COVID-19 Infection; Results of the Trinity Rheumatology and Covid-19 Registry – TRACR [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/anticytokine-therapies-for-inflammatory-rheumatic-disease-ird-are-associated-with-reduced-hospitalisation-following-community-covid-19-infection-results-of-the-trinity-rheumatology-and-covid-19-reg/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/anticytokine-therapies-for-inflammatory-rheumatic-disease-ird-are-associated-with-reduced-hospitalisation-following-community-covid-19-infection-results-of-the-trinity-rheumatology-and-covid-19-reg/