Session Information
Date: Tuesday, November 14, 2023
Title: (2257–2325) SLE – Diagnosis, Manifestations, & Outcomes Poster III
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Real-world data assessing the effectiveness of the anti-SARS-CoV2 vaccination in patients living with systemic lupus erythematosus (SLE) are currently lacking. We aimed to describe the uptake of the anti-SARS-CoV2 vaccination in 2021 and to investigate its clinical effectiveness in SLE patients living in Sweden.
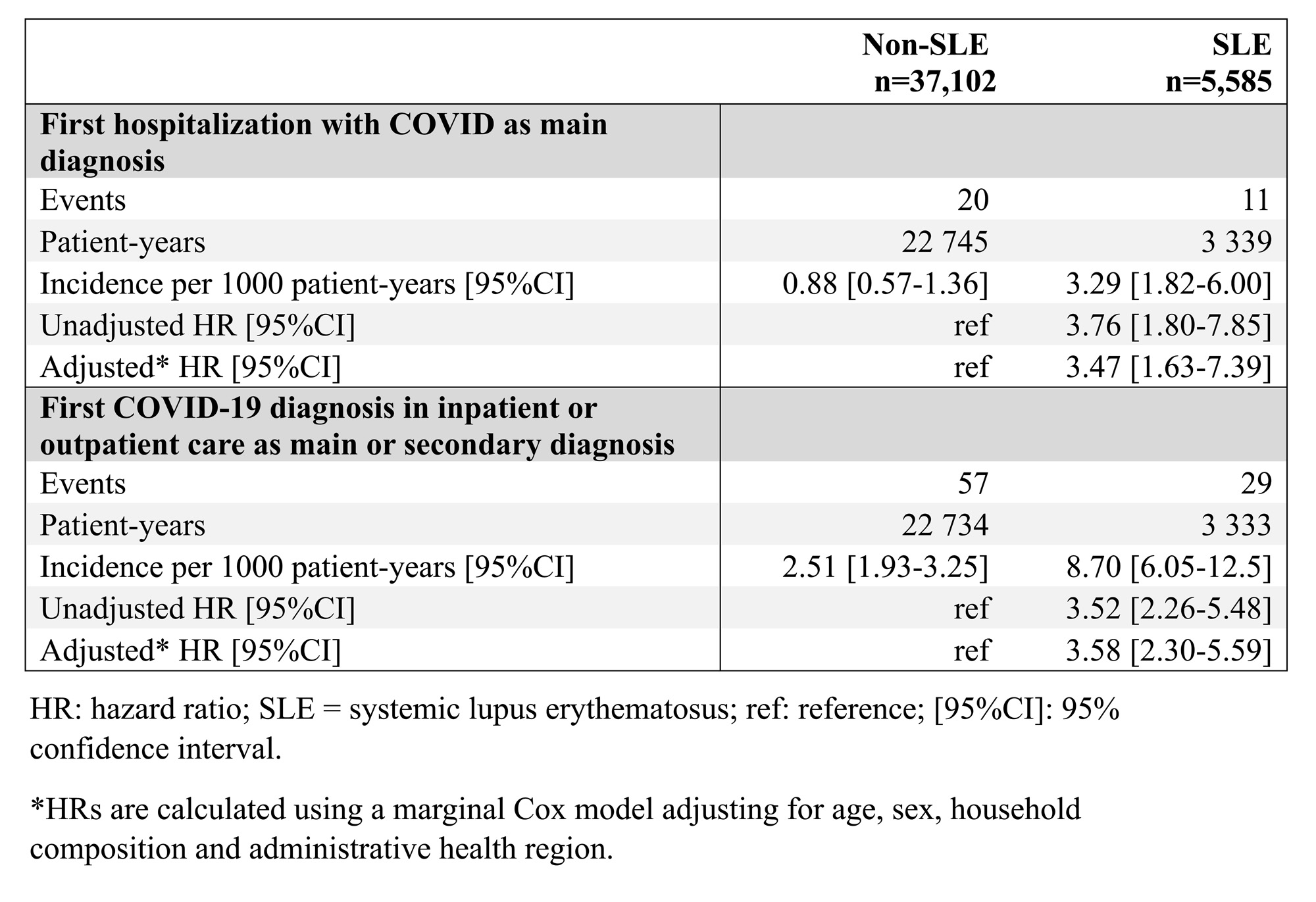
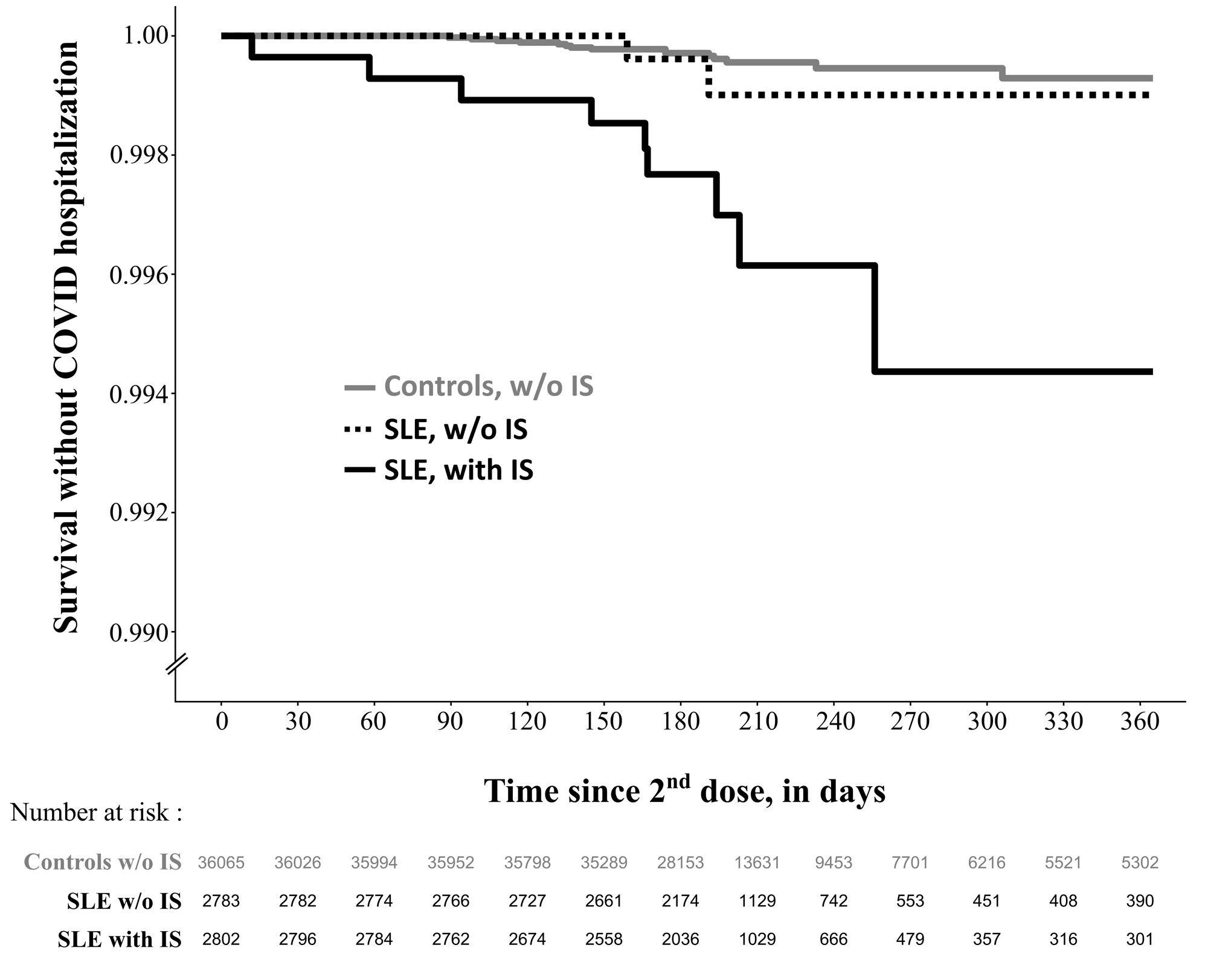
Methods: First, we described the cumulative incidence of first anti-SARS-CoV2 vaccination among SLE patients and matched comparators living in Sweden on January 1, 2021 using the nationwide Swedish National Patient Register (NPR) and the National Vaccination Register. To assess vaccine effectiveness, we restricted the population to SLE patients and comparators i) with no COVID-19 diagnosis code before the 2nd vaccine dose and ii) who received two doses of anti-SARS-CoV2 mRNA vaccines before January 1st, 2022. The main outcome was a first hospitalization with COVID-19 as main diagnosis in the NPR. The secondary outcome was defined as first COVID-19 diagnosis in inpatient or outpatient care, as main or secondary diagnosis. Rates of main and secondary outcomes were compared between SLE patients and comparators. Multivariable-adjusted marginal Cox models estimate hazard ratios and 95% confidence intervals (HR;95%CI) overall and stratified by immunosuppressive (IS) treatment received during the year before second vaccine dose.
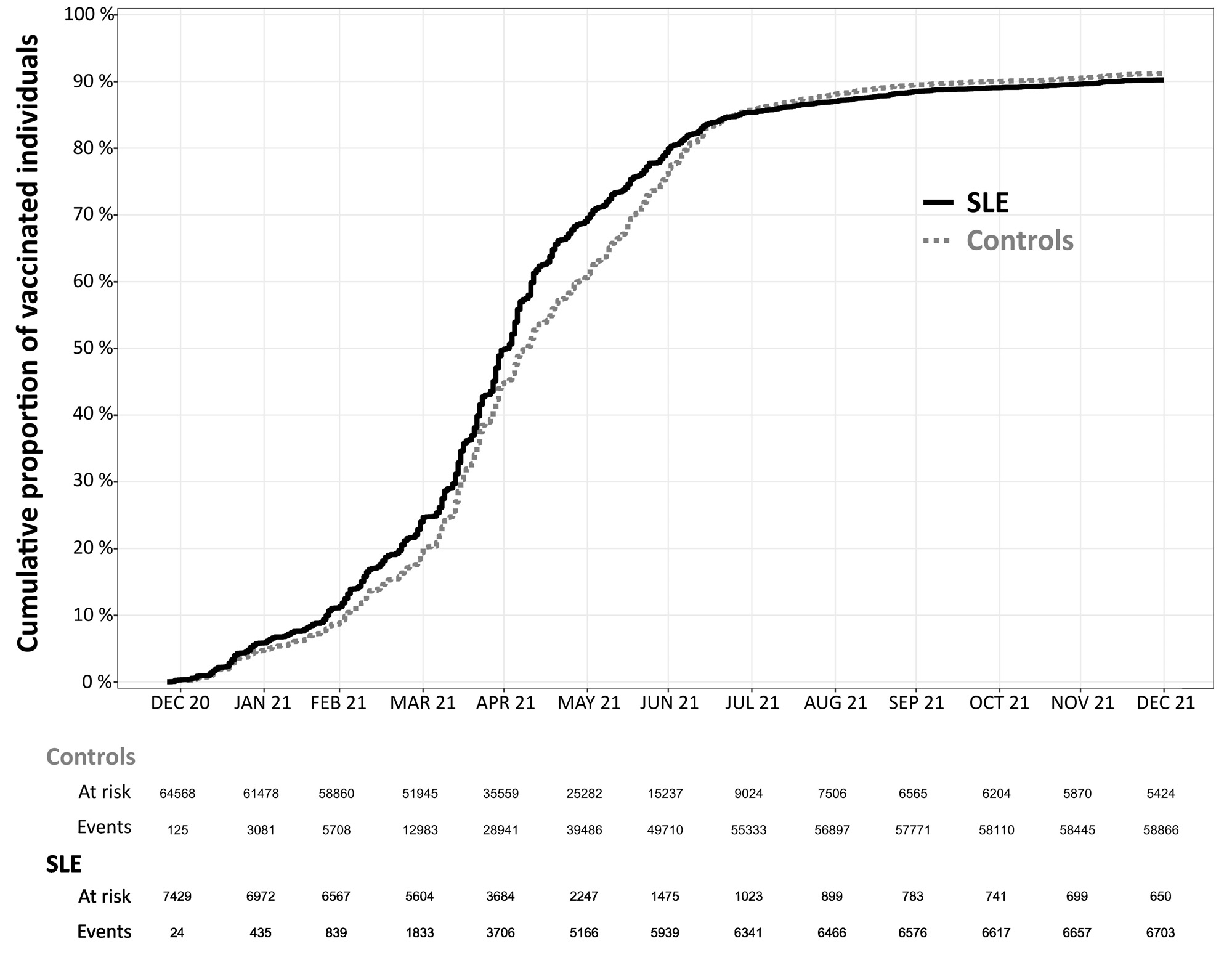
Results: To describe the vaccine coverage, we included 7,429 SLE patients and 64,568 comparators matched on age, sex and county of residence. Vaccination uptake was similar over 2021 between SLE patients and comparators (Figure 1). By the end of 2021, around 10% of both SLE and comparators received no vaccine doses. Among 5,585 SLE patients and 37,102 comparators included in the effectiveness analysis, we observed 11 hospitalizations with COVID-19 listed as the primary diagnosis in the SLE group and 20 in the comparator group (Table 1). SLE was associated with a higher risk of COVID-19 hospitalization (HR 3.47; 95%CI 1.63-7.39). Rates of events were higher in both groups using the secondary outcome (SLE N=29, comparators N=57) but the HR was similar to the main outcome (HR 3.58; 95%CI 2.30-5.59). There were 2,802 SLE patients (50.2%) who were treated with IS during the year before second vaccine dose. The HR of COVID-19 hospitalization was higher for IS-treated SLE (HR 7.03; 95%CI 3.00-16.5) than for IS-untreated (HR 1.50; 95%CI 0.34-6.60; Figure 2) compared to the general population.
Conclusion: Anti-SARS-CoV2 vaccination coverage was similar between SLE patients and the general population in Sweden, but it could still be improved. Even though the incidence of post-vaccination COVID-19 hospitalization was very low, vaccine effectiveness was diminished in SLE patients and lowest in those treated with immunosuppressants.
To cite this abstract in AMA style:
Mageau A, Simard J, Svenungsson E, Arkema E. Anti-SARS-CoV-2 Vaccination Among Patients Living with Systemic Lupus Erythematosus in Sweden: Coverage and Clinical Effectiveness [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/anti-sars-cov-2-vaccination-among-patients-living-with-systemic-lupus-erythematosus-in-sweden-coverage-and-clinical-effectiveness/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/anti-sars-cov-2-vaccination-among-patients-living-with-systemic-lupus-erythematosus-in-sweden-coverage-and-clinical-effectiveness/