Session Information
Session Type: ACR Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose :
Autoantibodies are important biomarkers in the diagnosis of idiopathic
inflammatory myopathies (IIM) including polymyositis (PM) and dermatomyositis
(DM), inclusion body myositis (IBM) as well as overlap syndromes. Recently, it
was reported that the prevalence of necrosis in patients with IIM is increasing
and that the majority of the patients with necrosis exhibit autoantibodies to
3-hydroxy-3-methylglutaryl-coenzyme A reductase
(HMGCR), the molecular target of statins. This is the first international
multi-center study on anti-HMGCR antibodies in a large cohort of patients.
Methods:
A total of 1906 samples from IIM patients and controls were collected
at 12 different sites from nine different countries. Among patients with IIM
(n=1250), 69 had immune mediated necrotizing myopathies (IMNM), 406 had PM, 525
had DM, 10 had PM/Scleroderma overlap syndrome, 45 had juvenile dermatomyositis
(JDM), 18 had myositis overlap syndromes (MOS), 53 had amyopathic
dermatomyositis (ADM), 49 had antisynthetase syndrome
(ASS), 64 had cancer-associated myositis and 11 had IBM. All samples were
tested for anti-HMGCR antibodies by ELISA.
Results:
Anti-HMGCR antibodies were present in 44.9% of IMNM, 4.4% of PM, 1.9% of DM, 6.7% of JDM, in 1.2% of primary Sjögren`s syndrome (pSS) and in 0.4%
of systemic lupus erythematosus patients
(see Table 1).
Table 1 Prevalence of anti-HMGCR antibodies in different
disease cohorts
|
Disease Group |
N= |
Prevalence |
95% CI |
|
Immune Mediated Necrotizing Myopathy (IMNM) |
31/69 |
44.9% |
33.8-56.6% |
|
Polymyositis (PM) |
18/406 |
4.4% |
2.8-6.9% |
|
Dermatomyositis (DM) |
10/525 |
1.9% |
1.0-3.5% |
|
Juvenile Dermatomyositis (JDM)
|
3/45 |
6.7% |
2.3-17.9% |
|
Primary Sjögren’s Syndrome (pSS)
|
1/81 |
1.2% |
0.02-6.7% |
|
Systemic Lupus Erythematosus (SLE) |
1/226 |
0.4% |
0.01-2.5% |
Among the IMNM patients, statin exposure was known for 45 patients. Patients
tested positive for the anti-HMGCR were more frequently statin users (21 vs.
10; p<0.0001), showed a higher
prevalence of necrosis (p<0.0001)
and were older (p=0.0001) compared to
ant-HMGCR negative patients. Receiver operating characteristic analyses showed
good discrimination between IMNM and controls, and between IMNM and other forms
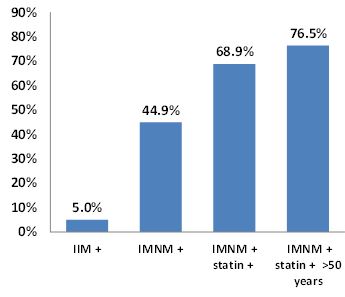
of IIM. The prevalence of anti-HMGCR antibodies was highest in statin exposed
elderly individuals (>50 years) diagnosed as IMNM reaching 76.5%.
Figure 1 Incremental prevalence of anti-HMGCR antibodies in
different patient subsets
Conclusion:
Anti-HMCGR antibodies characterize a subpopulation of IMNM patients
previously exposed to statin and were significantly associated with an older
age. However, it is important to note that not all patients with those autoantibodies
had a history of exposure to statins indicating that different phenotypes and
mechanisms exist.
To cite this abstract in AMA style:
Musset L, Bentow C, Fritzler MJ, Vencovsky J, Benveniste O, Garcia de la Torre I, Franceschini F, Danko K, Peng Q, Hue S, Boyer O, Bizzaro N, Muro Y, Bossuyt X, Ghirardello A, Mahler M. Anti-Hmgcr Antibodies As Specific Marker for Immune Mediated Necrotizing Myopathies [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/anti-hmgcr-antibodies-as-specific-marker-for-immune-mediated-necrotizing-myopathies/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/anti-hmgcr-antibodies-as-specific-marker-for-immune-mediated-necrotizing-myopathies/