Session Information
Date: Monday, November 13, 2023
Title: (1554–1578) Vasculitis – Non-ANCA-Associated & Related Disorders Poster II
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Takayasu’s arteritis (TAK) is an autoimmune disease that primarily affects the aorta and its major branches. It has an incidence of 1-3 per million people in the USA and Europe and is primarily seen in females between the ages of 10 – 40 years. Coronary artery involvement has been reported in TAK. This study aims to analyze TAK as a risk factor for acute coronary syndrome (ACS) in a US inpatient population.
Methods: We conducted a retrospective review of 2016-2020 National Inpatient Sample (NIS) database. All adult hospitalizations were selected as our study population and were subdivided into those with and without ACS (ICD-10 codes I20 and I21). For ACS risk factors, the following ICD-10 codes were used: diabetes (DM) code E08-E13, hypertension (HTN) code I10, hyperlipidemia (HLD) code E78, and obesity code E66. A univariable analysis was used to calculate unadjusted odds ratios (ORs) for ACS. All variables with p values ≤ 0.2 were included in a multivariable logistic regression model with p values < 0.05 considered to be significant.
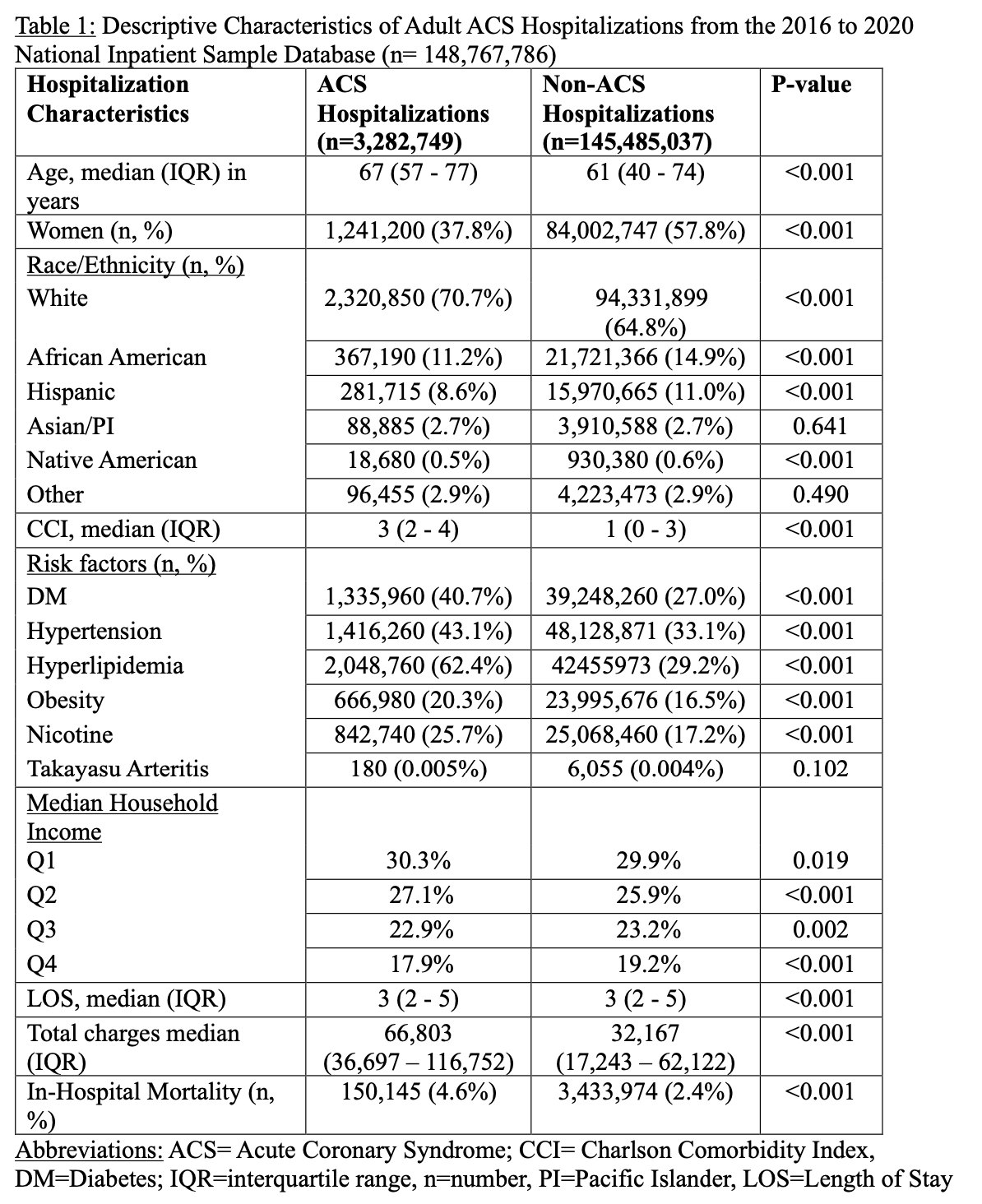
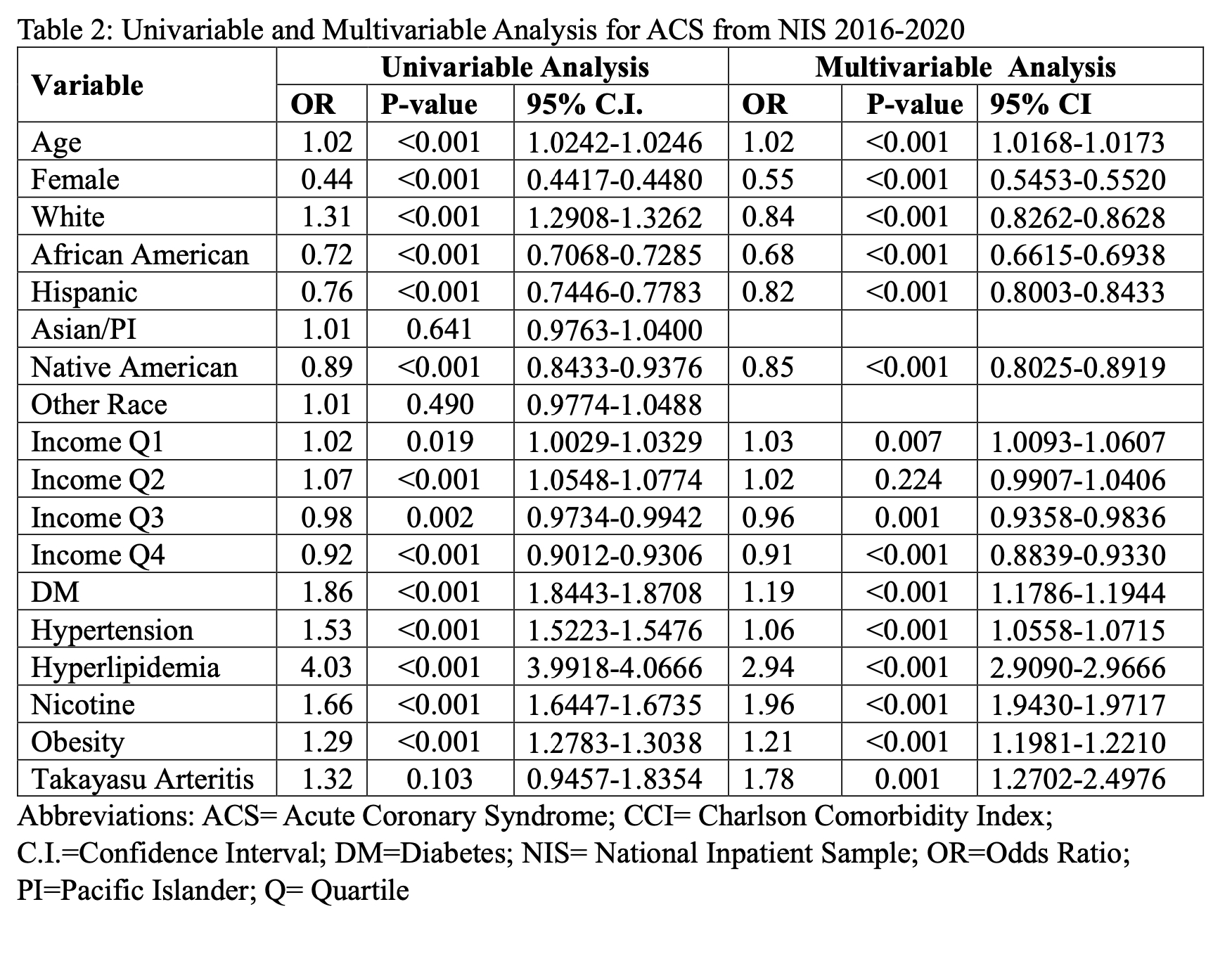
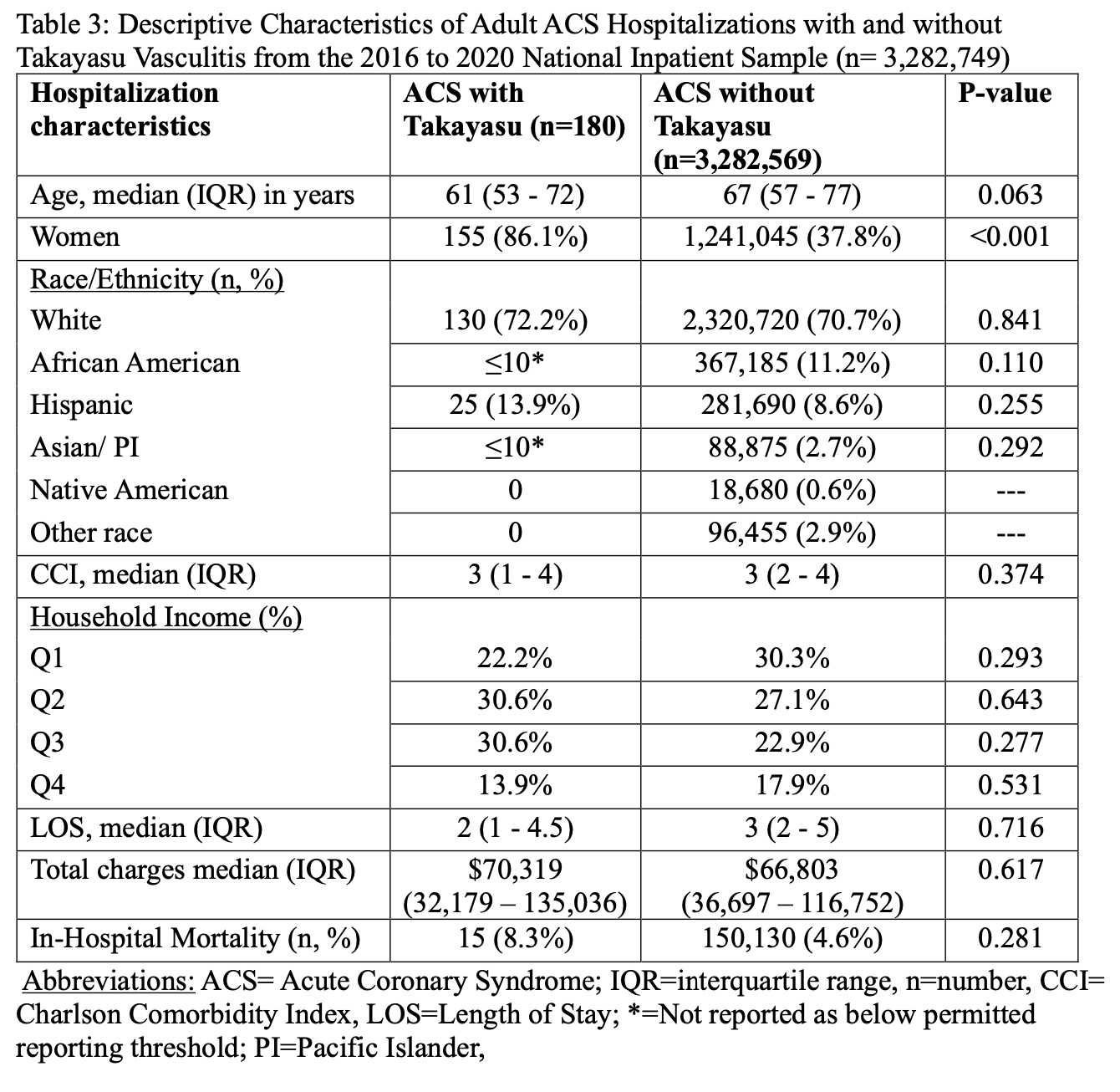
Results: There were 148,767,786 adult hospitalizations in the 2016 to 2020 NIS database. Of those, 3,282,749 of those had a primary diagnosis of ACS. Compared to non-ACS hospitalizations (Table 1), the ACS group was older (median age 67 vs 61 years; p< 0.001), had less females (37.8% vs 57.8%; p< 0.001), more Whites (70.7% vs 65.8%; p< 0.001), less African Americans (11.2% vs 14.9%; p< 0.001), less Hispanics (8.6% vs 11%; < 0.001), same Asian/Pacific Islander (2.7% vs 2.7%; p=0.641), less Native Americans (0.5% vs 0.6%; p< 0.001), higher CCI (3 vs 1; < 0.001), lower household income, higher median total hospital charges ($66,803 vs $32,167; p< 0.001) and higher in-hospital mortality (4.6% vs 2.4%; p< 0.001). LOS was similar between the ACS and non-ACS hospitalizations. Univariable analysis for the outcome of ACS showed that age, white race, lowest income quartile, DM, HTN, HLD, obesity, nicotine dependence/tobacco use and TAK were associated with higher odds of ACS (Table 2). Female, African American race, Hispanic race, Native American race and upper two income quartiles were associated with a lower odds of ACS. Multivariable analysis showed that age (OR 1.02; 95% C.I. 1.0168 – 1.0173), lowest income quartile (OR 1.03; 95% C.I. 1.0093 – 1.0607), DM (OR 1.19; 95% C.I. 1.1786 – 1.1944), HTN (OR 1.06; 95% C.I. 1.0558 – 1.0715), HLD (OR 2.94; 95% C.I. 2.9090 – 2.9666), obesity (OR 1.21; 95% C.I. 1.1981 – 1.2210), nicotine dependence/tobacco use (OR 1.96; 95% C.I. 1.9430 – 19717) and TAK (OR 1.78; 95% C.I. 1.2702 – 2.4976) were associated with higher odds of ACS (Table 2). In comparison to ACS without TAK, ACS with TAK group comprised of more females (86.1% vs 37.8%; p< 0.001) and showed a trend towards being younger (Table 3).
Conclusion: We performed an analysis of the 2016-2020 NIS database to better understand TAK as a risk factor for ACS. After controlling for traditional ACS risk factors, TAK was found to increase the odds of ACS by 1.78 times. Other significant ACS risk factors from the multivariable analysis included age, low income, DM, HTN, HLH, obesity, and nicotine dependence. This study emphasizes the importance of recognizing TAK as a risk factor for ACS especially in women and in the younger population.
To cite this abstract in AMA style:
Romero Noboa M, Arora S, Manadan A. Analysis of Takayasu’s Arteritis as Risk Factor for Acute Coronary Syndrome [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/analysis-of-takayasus-arteritis-as-risk-factor-for-acute-coronary-syndrome/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/analysis-of-takayasus-arteritis-as-risk-factor-for-acute-coronary-syndrome/