Session Information
Date: Monday, November 14, 2022
Title: SLE – Diagnosis, Manifestations, and Outcomes Poster III: Outcomes
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: Lupus can present as either systemic lupus erythematous (SLE) and/or a cutaneous form known as cutaneous lupus erythematous (CLE). While a lot of data exists on SLE hospitalization, large population studies on CLE hospitalizations are limited. We aim to determine the most common reasons for hospitalization of patients with CLE. We also aim to compare baseline demographic and hospital outcomes of hospitalizations of patients with CLE (without any systemic manifestations) and patients with SLE with organ involvement.
Methods: The National Inpatient Sample (NIS) is the largest inpatient all-payer public database in the United States (US). We obtained data from the NIS 2016-2019 databases. For the CLE cohort, we abstracted data for patients aged ≥18 years with any diagnosis of CLE, using the ICD-10 code “L93”. CLE cohort includes patients with discoid lupus erythematosus, subacute cutaneous lupus erythematosus, lupus erythematosus profundus, and lupus panniculitis. We excluded patients with any form of SLE using ICD-10 code “M32” from the CLE cohort. For comparison, we obtained the SLE cohort by searching for patients aged ≥18 years with any diagnosis of SLE with organ involvement using ICD-10 code “M321”. Analyses were performed using STATA, version 16. By using a “rank” command in STATA, the most common principal discharge diagnoses were divided into categories based on organ system, and the most common specific principal discharge diagnoses were recorded for the CLE cohort in descending order of frequency. We used chi-square test to compare baseline demographic characteristics between the CLE and SLE cohorts. We used multivariable logistic and linear regression analysis, adjusting for gender, age, Charlson comorbidity index score (CCI), insurance status, and income for categorical and continuous hospital outcomes respectively between both cohorts.
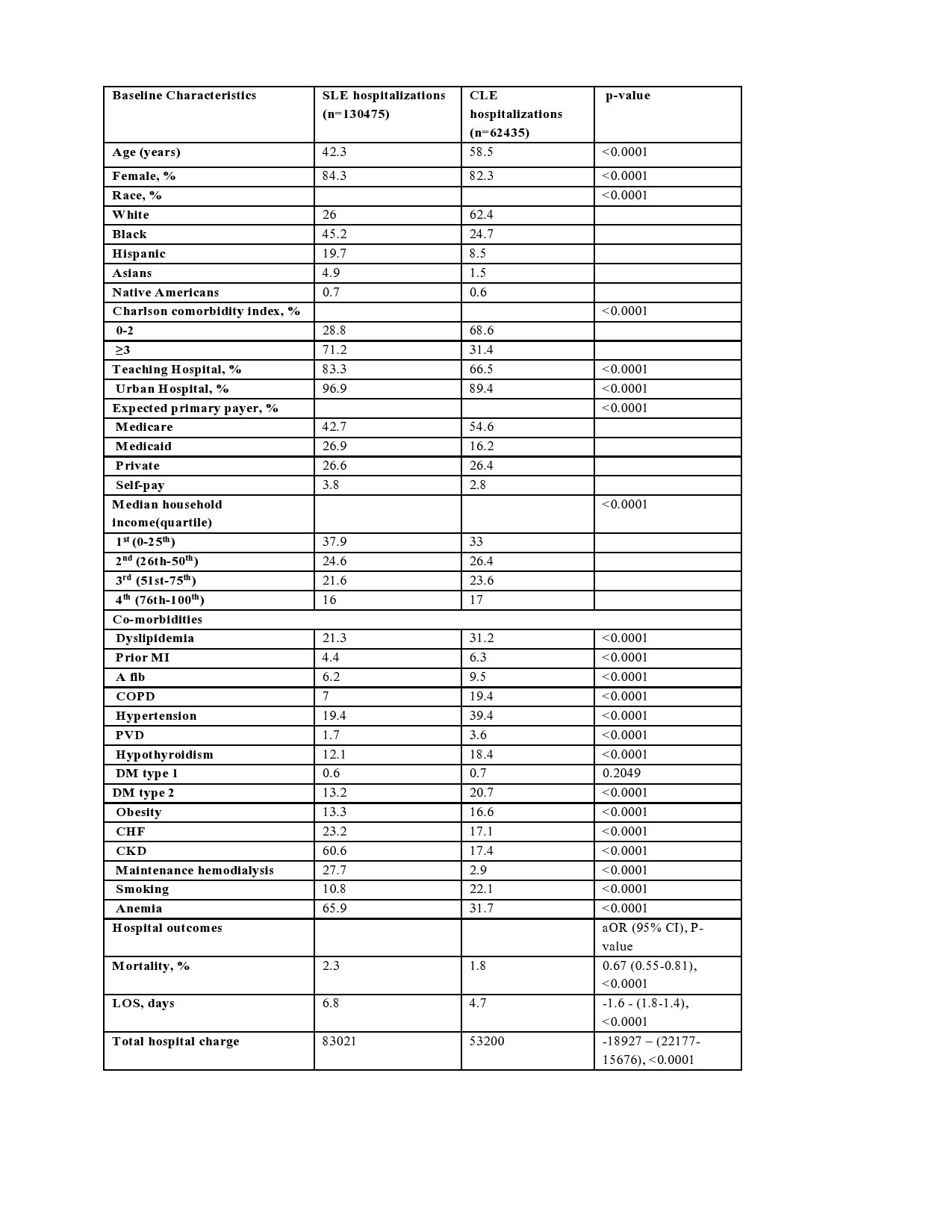
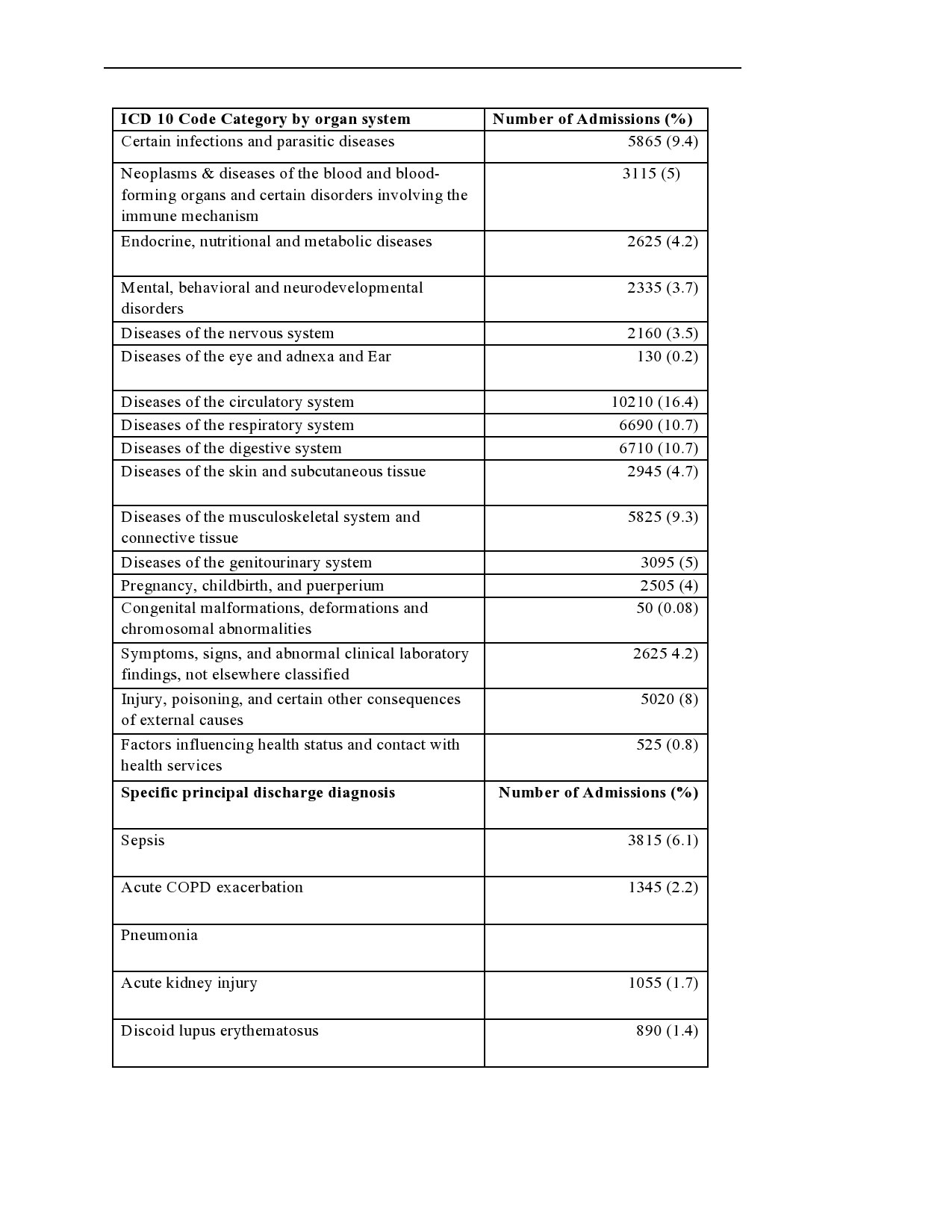
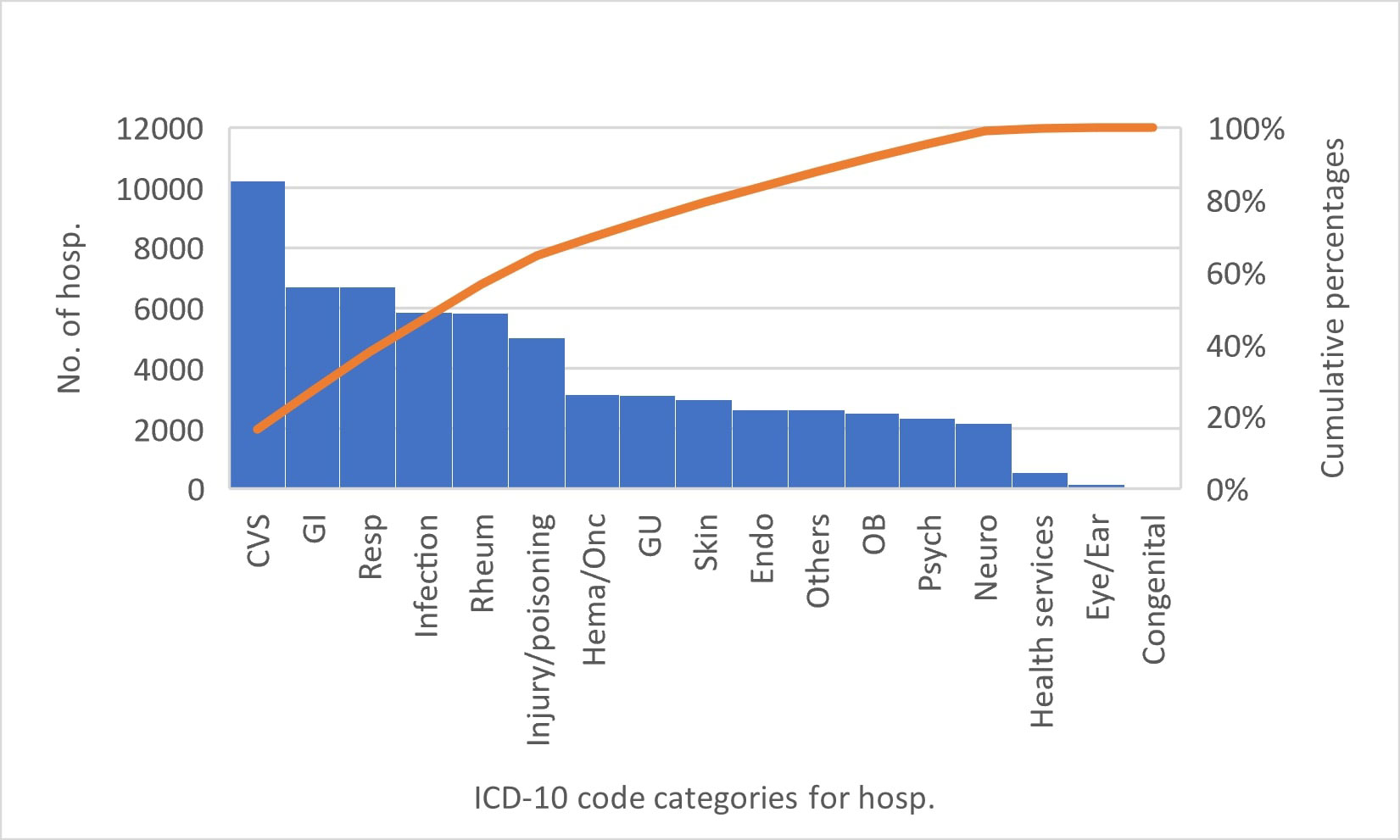
Results: About 142 million hospitalizations were included in the combined NIS databases, out of which the SLE cohort contained 130,475 hospitalizations (0.09%) while the CLE cohort contained 62,435 hospitalizations (0.04%). The CLE cohort was older, had fewer females, lower inpatient mortality, shorter hospital length of stay (LOS), less total hospital charges, less CCI, more whites, and fewer racial minorities compared to the SLE cohorts (Table 1). The CLE cohort had more cardiovascular (CV) risk factors such as dyslipidemia, prior myocardial infarction, hypertension, peripheral vascular disease, type 2 diabetes, obesity, and smoking compared to the SLE cohort. The most common principal diagnosis category of hospitalizations of patients with CLE was CV (Figure 1), while the most common specific principal diagnosis for these patients was sepsis (Table 2).
Conclusion: Hospitalized CLE patients differ significantly from SLE patients in terms of socio-demographics, comorbidities, and hospital outcomes. Management of comorbidities (such as CV), and measures to prevent and early detection of infections in the outpatient are necessary in reducing hospitalizations of these patients.
Abbreviations
CLE: Cutaneous lupus erythematosus, SLE: Systemic lupus erythematosus with organ or systemic involvement, MI: Myocardial infarction, PCI: percutaneous coronary intervention, CABG: Coronary artery bypass graft, COPD: Chronic obstructive pulmonary disease, DM: Diabetes Mellitus, CHF: Chronic congestive heart failure, CKD: Chronic kidney disease, O2: oxygen, A. Fib: Atrial fibrillation, median household income: median household income for patient’s Zip code, Co-morbidities: Secondary diagnosis present at admission or developed during hospitalization, aOR, CI: 95% CI: 95% confidence interval
* Hospitalizations for patients with principal or secondary diagnosis of cutaneous lupus erythematosus. COPD: Chronic obstructive pulmonary disease. CKD: Chronic kidney disease, HF: Heart failure
Abbreviations: Hema/Onc: Neoplasms & diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism, Endo: Endocrine, nutritional and metabolic diseases, Psych: Mental, behavioral and neurodevelopmental disorders, Neuro: Diseases of the nervous system, CVS: Diseases of the circulatory system, Respiratory: Diseases of the respiratory system, GI: Diseases of the digestive system, Rheum: Diseases of the musculoskeletal system and connective tissue, GU: Diseases of the genitourinary system, others: Symptoms, signs, and abnormal clinical laboratory findings, not elsewhere classified, Health services: Factors influencing health status and contact with health services
To cite this abstract in AMA style:
Edigin E, Trang A, Osuorji C, Hino C, Anighoro S, Eseaton P, Chukwu N, Aihie O, Manadan A, Sandhu v. Analysis of Cutaneous Lupus Hospitalizations: A United States National Population-based Study [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/analysis-of-cutaneous-lupus-hospitalizations-a-united-states-national-population-based-study/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/analysis-of-cutaneous-lupus-hospitalizations-a-united-states-national-population-based-study/