Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Osteoporosis is a widely recognized disease of the bone where bone mineral density is decreased leading to increased risk for fracture. Bone mineral density seen on dual-energy x-ray absorptiometry (DXA) is the standard test for osteoporosis. There are clear recommendations for screening with DXA in post-menopausal females; the Endocrine Society and USPSTF recommend screening all post-menopausal women or women over the age of 65. However, there are not clear screening guidelines for men; the Endocrine Society recommends osteoporosis screening in men over the age of 70 or men ages 60-69 with risk factors such as delayed puberty, hypogonadism, hyperparathyroidism, hyperthyroidism, chronic obstructive pulmonary disease, alcohol abuse, and smoking. The USPSTF does not outline clear guidelines for DXA screening in men. The aim of this quality improvement project is to evaluate patients hospitalized with a fragility fracture, captured in the Lehigh Valley Health Network Fracture Database, and assess the compliance and discrepancy of bone density screening and treatment based on gender. We hypothesized that male patients who sustained a fragility fracture are under-screened for osteoporosis, leading to increased risk for subsequent fractures.
Methods: We collected and analyzed the records of patients from an established database within our network; we identified 2680 patients within LVHN who were diagnosed with a fragility fracture between the dates of 1/1/2022 – 1/1/2024. Using the Endocrine society guidelines listed above, we compared the compliance of DXA screening and osteoporosis treatment within men over 70 years of age with women over 65 years of age. Other secondary risk factors were not taken into account in this project.
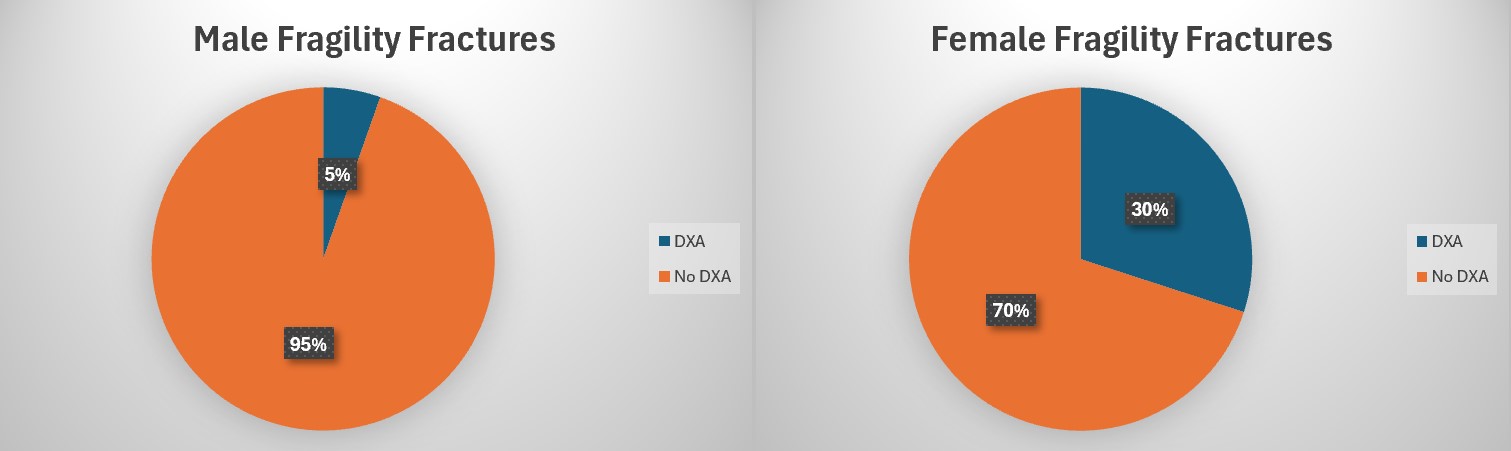
Results: Of the 2680 patients, 703 men and 1977 women were identified as having a fragility fracture. Of the 703 men, 38 men (5.4%) had a completed DXA scan within 2 years prior to or 6 months following the date of fracture. Of the 1977 women, 593 women (30.0%) had a completed DXA scan within 2 years prior to or 6 months following the fracture. (Figure 1).
Conclusion: As expected, a higher percentage of women compared to men suffered a fragility fracture. However, this was followed by a marked discrepancy in rates of DXA screening between the two genders with 5.4% of men and 30% of women being noted to have completed DXAs. While women are at an increased risk for osteoporosis, our analysis indicates that more than one-third of fragility fractures occurred in men, of which only 5% had a bone density screening. We suspect that the lack of consensus among osteoporosis screening guidelines and lack of clarity of appropriate ICD diagnostic code coverage for DXA screening in men may contribute to decreased screening in this population. The low rate of DXA screenings done after a fragility fracture is the primary area of focus for the LVH Bone Health Initiative Program in order to capture this high-risk population for treatment of osteoporosis and reduction of recurrent fractures. This project highlights the need for increased osteoporosis screening for men, not only based on age recommendations, but also on other risk factors when screening a high-risk population.
To cite this abstract in AMA style:
Wolff B, Bigelsen R, Zaffiri K, Kim S, Dunn P. An Analysis of Osteoporosis Screening in Males vs. Females Across Lehigh Valley Health Network [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/an-analysis-of-osteoporosis-screening-in-males-vs-females-across-lehigh-valley-health-network/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/an-analysis-of-osteoporosis-screening-in-males-vs-females-across-lehigh-valley-health-network/