Session Information
Date: Monday, November 9, 2015
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Environmental risk factors, such as
air pollution, have been studied in relation to the risk of development of
rheumatic diseases, including rheumatoid arthritis (RA), systemic autoimmune
rheumatic diseases (SARDs), vasculitis and juvenile
idiopathic arthritis (JIA). We have performed a systematic literature and
meta-analysis to summarize the existing knowledge.
Methods: Medline (1950 to May 2015) and EMBASE (1980 to May
2015) databases and rheumatology conference abstracts (2012-2015) were searched
using MeSH terms and keywords to identify cohort and
case-control studies reporting risk estimates (hazard ratios, relative risks,
odds ratios) for the development of select rheumatic diseases in relation to
exposure to measured air pollutants. Meta-analysis was completed using the
generic inverse-variance approach with random effects models using RevMan version 5.3.
Results: A total of 103 non-overlapping publications were
identified of which 20 underwent full-text review, with 9 studies included in
qualitative synthesis and 2 studies used for meta-analysis. Three studies
included subjects with RA (one cohort study, two case-control studies) and
examined associations with exposure to nitrogen dioxide (NO2), sulfur
dioxide (SO2) and particulate matter up to 10 micrometers in size
(PM10). An association with particulate matter up to 2.5 micrometers
in size (PM2.5) was studied in the RA cohort study, and additional
pollutants (carbon monoxide, nitrous oxide, ozone and black carbon) in one
case-control study. In the RA cohort study, there was no definite evidence for
increased RA risk related to NO2, SO2, PM10 or PM2.5 exposures. In the case-control studies, there was no evidence
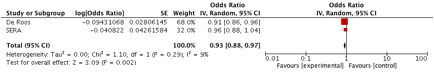
of an increased risk for the development of RA with exposure to NO2 (pooled OR
0.93, 95%CI 0.86 to 1.01) or SO2 (pooled OR 0.94, 95%CI 0.82 to 1.08), but possibly a
protective effect with exposure to PM10 (pooled OR
0.93, 95%CI 0.88 to 0.97, Figure 1). Both case-control studies in SARDs
indicated higher odds of having SARDs in relation to increasing PM2.5
exposure. Two studies examined vasculitis conditions
(ANCA vasculitis and PM10 exposure,
Kawasaki Disease and PM2.5 exposure) but were unable to draw definitive
conclusions regarding associations. One study of found an increased relative
risk for JIA related to PM2.5 exposure but only in American children <5.5 years
of age; the results were inconclusive when studying a broader JIA population in
America and Canada.
Conclusion: The existing studies do not support an association
between air pollutant exposures and the development of RA, SARDs, or vasculitis, and uncertain effects in JIA. The measurement of cumulative and time-varying exposures are
important considerations for future studies.
Figure 1. Meta-Analysis of
Association Between RA Development and PM10 Exposure
To cite this abstract in AMA style:
Sun G, Hazlewood G, Bernatsky S, Kaplan G, Eksteen B, Barnabe C. Air Pollution and the Rheumatic Diseases: A Systematic Review and Meta-Analysis [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/air-pollution-and-the-rheumatic-diseases-a-systematic-review-and-meta-analysis/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/air-pollution-and-the-rheumatic-diseases-a-systematic-review-and-meta-analysis/