Session Information
Date: Tuesday, November 14, 2023
Title: (2257–2325) SLE – Diagnosis, Manifestations, & Outcomes Poster III
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Patients with systemic lupus erythematosus (SLE) frequently visit the emergency department (ED) due to the complex disease course. Previous research highlights infection and pain as key reasons for ED use in SLE. Our previous study using the US National Emergency Department Sample (NEDS) found that SLE ED visits consisted of more young patients, of Black race, with publicly funded insurance and a higher comorbidity burden, but Black patients were less likely to be admitted from the ED. This study aims to further investigate age and race-based variations in ED utilization.
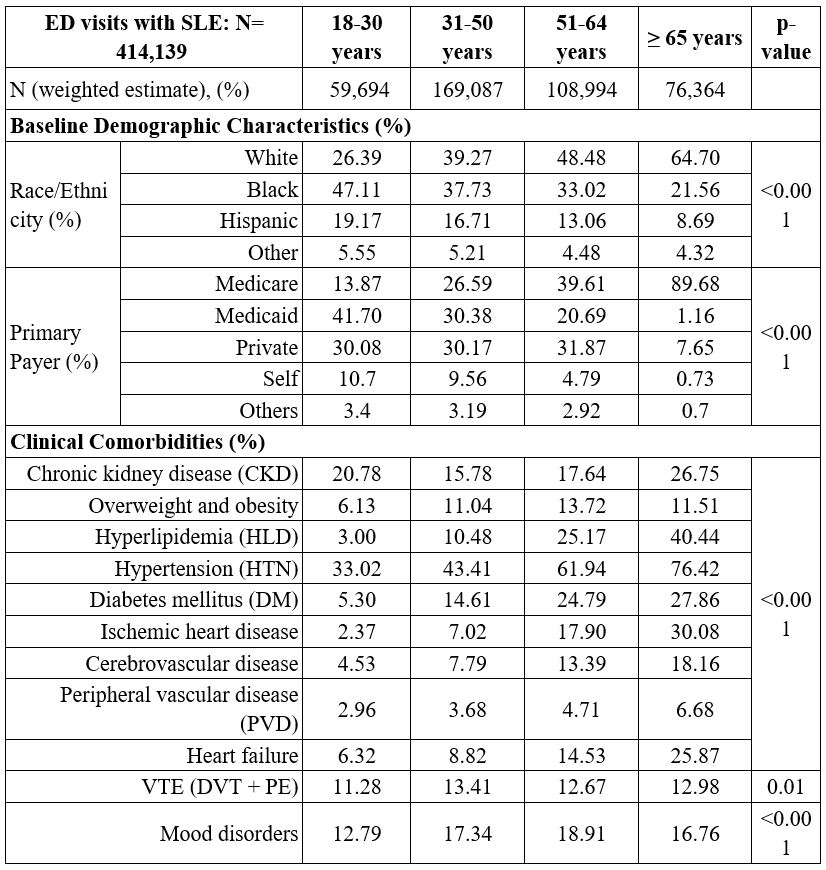
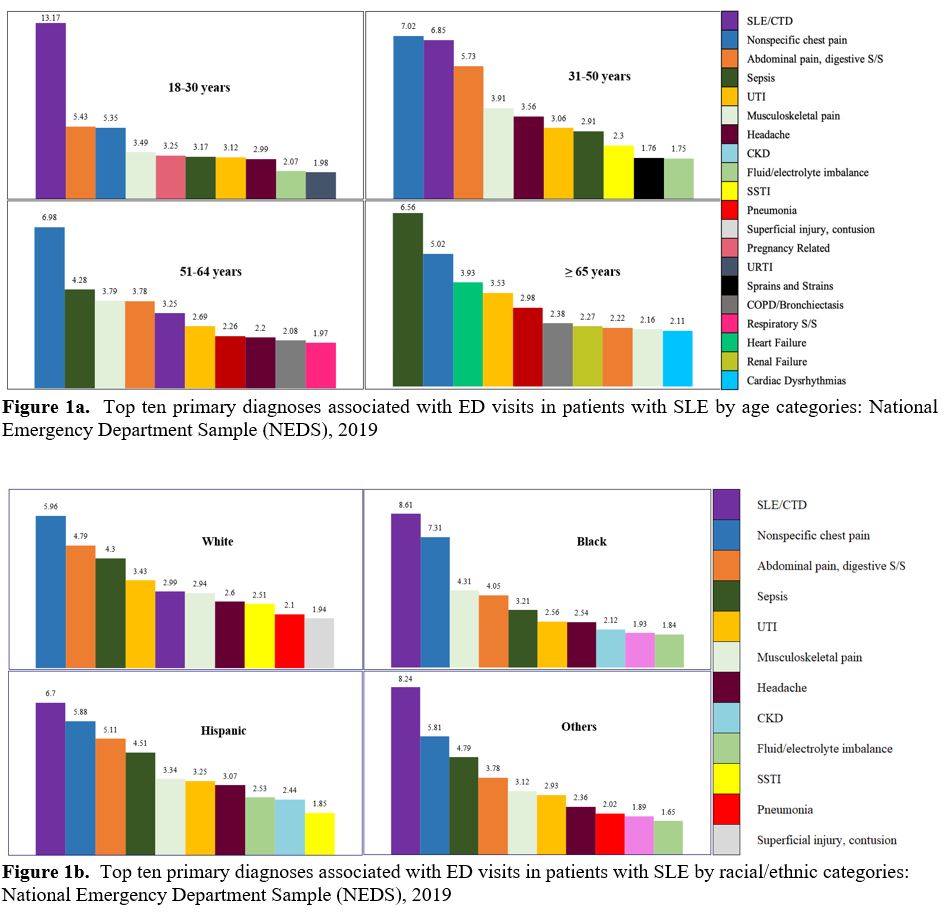
Methods: Using NEDS (2019) discharge data for 989 hospitals, which approximates a 20% sample of US hospital-owned EDs, SLE visits were identified using ICD-10 codes (M32.xx) and categorized by age (18-30, 31-50, 51-64, and ≥ 65 years) and race (White, Black, Hispanic, Others). Demographic features, clinical comorbidities, and the top ten primary diagnoses associated with ED visits were compared across groups.
Results: We identified 414,139 ED SLE visits, 41% of which were visits by adults aged 31-50 years. Young SLE adults (18-30 years) visiting the ED were predominantly Black (47.10%), and had Medicaid (41.70%), while older adults (≥ 65 years) were mostly White (64.70%). Older adults had higher rates of chronic kidney disease (CKD), hyperlipidemia (HLD), hypertension (HTN), diabetes, and cardiovascular diseases (CVDs), but young SLE adults (18-30 years) also exhibited significant comorbidity burdens (CKD: 20.78%, HTN: 33.02%). Analyzing by race, more ED visits by Black and Hispanic SLE patients were in the 18-30 age group (~20%) compared to White patients (< 10%). Medicaid use was notably higher among non-White (27-32%) versus 19% in White patients. Comorbidity patterns varied, with White patients having higher HLD, ischemic heart disease (IHD), and mood disorders while Black patients had higher CKD and HTN (25% vs 13% and 61% vs 48%, respectively). The most common primary diagnosis for ED visits in young SLE adults (18-31 years) was “SLE/Connective tissue disease (CTD)”, whereas sepsis was the most common diagnosis for older adults (≥ 65 years). Heart failure and arrhythmias were among the top 10 diagnoses for adults ≥ 65 years, but not in younger groups. The primary ED diagnosis of SLE/CTD was more common in Black (8.61%) and Hispanic (6.70%) than in White patients (2.99%), with no other major differences in other reasons for ED visits based on race.
Conclusion: In a previous study of general population ED visits, Black patients were less likely to be admitted from the ED, and our study suggested a similar pattern among SLE ED visits. Discriminating determinants appear to be younger age, higher Medicaid use, CKD, HTN, and heart failure amongst Black SLE patients, and higher prevalence of older age groups, and baseline CVDs among White patients. While it appears that increased age and/or more severe CVDs in the White patients may explain the disparate admission rates, further study is needed to confirm whether these discriminating factors are replicated in other datasets and whether other factors such as ED reliance as a primary source of care and insurance coverage affect the lower admission rate amongst Blacks.
To cite this abstract in AMA style:
Dhital R, Karageorgiou I, Pokharel A, Kalunian K. Age and Race-Based Differences in Emergency Department Utilization for Systemic Lupus Erythematosus in the United States [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/age-and-race-based-differences-in-emergency-department-utilization-for-systemic-lupus-erythematosus-in-the-united-states/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/age-and-race-based-differences-in-emergency-department-utilization-for-systemic-lupus-erythematosus-in-the-united-states/