Session Information
Date: Sunday, November 10, 2019
Title: 3S107: Pediatric Rheumatology – Clinical I: Systemic JIA (915–920)
Session Type: ACR Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: Macrophage activation syndrome (MAS) is a life-threatening complication of systemic juvenile idiopathic arthritis (sJIA) characterized by a vicious cycle of immune cell activation and dysregulated cytokine production that can result in multi-organ failure. Unambiguous biomarkers of MAS are needed to facilitate prompt diagnosis and treatment, as well as to inform the understanding of disease pathogenesis.
Methods: Adenosine deaminase 2 (ADA2) activity was quantified in peripheral blood using an established spectrophotometric assay in healthy children and in children with a range of inflammatory diseases. Sources of ADA2 and triggers for its release were explored using cytokine stimulation of peripheral blood mononuclear cells, flow cytometry, and confocal microscopy of MAS bone marrow.
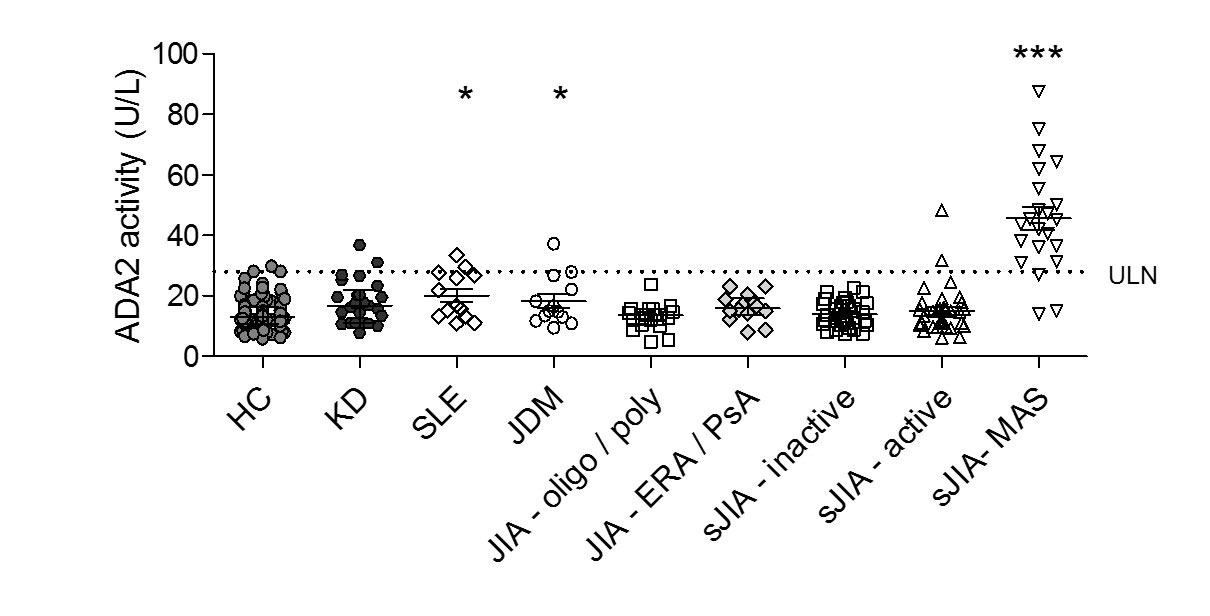
Results: We established normal levels of peripheral blood ADA2 levels in 175 healthy children and compared these values with Kawasaki disease (KD; n = 25), systemic lupus erythematosus (SLE; n = 13), juvenile dermatomyositis (JDM; n = 13) and multiple forms of juvenile idiopathic arthritis (JIA; n = 120). Aside from mild elevation in some patients with SLE and JDM, levels of ADA2 levels above the upper limit of normal were largely restricted to sJIA patients with clinically diagnosed MAS (Figure 1). In two independent sJIA cohorts, ADA2 activity beyond the upper limit of normal effectively distinguished MAS from active sJIA without MAS, with combined sensitivity = 86% and specificity = 93%. Longitudinal analysis of several patients with sJIA/MAS showed normalization of ADA2 levels with resolution of MAS. In sJIA patients, ADA2 levels correlated closely with other biomarkers of MAS including ferritin, interleukin (IL)-18, and the interferon (IFN)-γ-inducible chemokine CXCL9. In peripheral blood mononuclear cells, ADA2 was strongly induced by IL-12, IL-18 and IFN-γ. Monocytes were the primary ADA2 source in peripheral blood, with hemophagocytes a prominent source of ADA2 in MAS bone marrow as assessed by confocal microscopy.
Conclusion: ADA2 in the peripheral blood is a sensitive and specific biomarker of MAS, reflecting the activation status of monocytes, macrophages, and potentially hemophagocytes. In patients with active sJIA, ADA2 activity beyond the upper limit of normal represents strong evidence for concomitant MAS and could potentially help guide clinical care.
To cite this abstract in AMA style:
Lee P, Schulert G, Canna S, Huang Y, Sundel J, Son M, Henderson L, Nigrovic P, Newburger J, Dedeoglu F, Lo M, Meidan E, Li Y, Halyabar O, Chang M, Hoyt K, Do T, Sundel R, Blaustein R. Adenosine Deaminase 2 as a Circulating Biomarker of Macrophage Activation Syndrome [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/adenosine-deaminase-2-as-a-circulating-biomarker-of-macrophage-activation-syndrome/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/adenosine-deaminase-2-as-a-circulating-biomarker-of-macrophage-activation-syndrome/