Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: There is lack of appropriate outpatient follow-up (F/U) for hospitalized rheumatology patients, which can result in disease recurrence and recurrent inpatient admissions1. This is a financial burden on the healthcare system due to unnecessary hospital admissions and emergency room visits2. Inpatients are often started on high risk medications. Due to lack of F/U in management, they may be at risk of developing adverse events.
Methods: We initiated an IRB-approved retrospective analysis on all hospitalized patients at an urban academic medical center who underwent a rheumatology consultation from 7/17/2017 – 8/31/2017, and whom were expected to follow up in clinic. Tabulated data for each patient included whether the patient followed up within 2 weeks of their expected appointment along with several variables. We subsequently conducted a prospective intervention study for all consulted inpatients during 2/1/2019 – 3/15/2019, which involved: 1) Each patient was explained the importance of F/U (particularly skilled nursing facility (SNF) patients). 2) A business card was provided with appointment date and time. 3) The consult team assured that administrative staff contacted each patient for a convenient appointment if unable to be made during hospitalization before discharge. 4) Disease-specific handouts were given to each patient, particularly gout patients. 5) Financial barriers were addressed by an inpatient social worker, and the option to follow up at satellite campuses was offered. Retrospective analysis was then repeated on data from this intervention group.
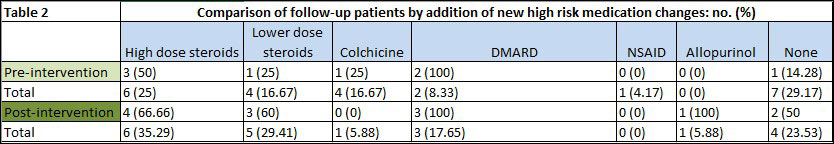
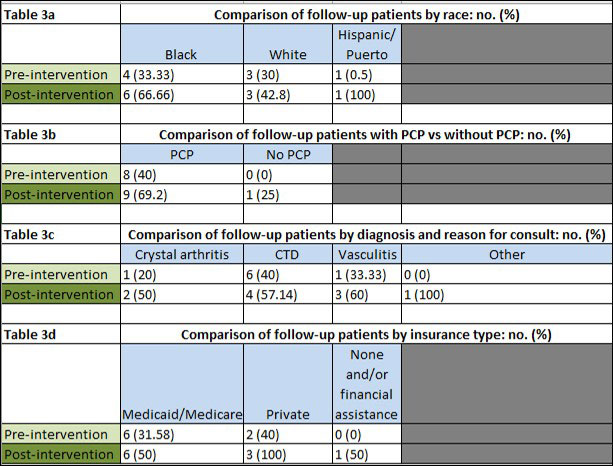
Results: The pre-intervention group had an overall low percentage of F/U (33%). Important contributors to low follow up included: patients without an established rheumatologist (18%), patients with no appointment made for F/U (29%), and patients discharged to a SNF (11%).
The post-intervention group (versus the pre-intervention group) had a higher percentage of post-discharge F/U for all patients (58% vs 33%). The post-intervention group F/U rate was also higher for the following: patients without repeat admission (66% vs 40%), scheduling of F/U appointment before discharge (62% vs 25%), patients without established rheumatologist (50% vs 18%), and patients discharged to SNF (66% vs 11%). Interestingly, among specific diseases analyzed (CTD, vasculitis, other), patients admitted for crystal-induced arthritis had the greatest improvement in F/U rate (50% vs 20%). All other categories examined showed improvement in the post-intervention group F/U rate as well.
Conclusion: A systems-based intervention is effective in improving outpatient follow up for hospitalized rheumatology patients. Particular focus should be on patient education, addressing financial and transportation barriers, and arranging follow up before discharge, all in a protocolized manner.
References
- Jackson C, et al. Timeliness of Outpatient Follow-up: An Evidence-Based Approach for Planning After Hospital Discharge. Ann Fam Med Mar 2015 vol. 13 no. 2 115-122.
- Thomas EJ, et al. Patient noncompliance with medical advice after the emergency department visit. Ann Emerg Med. 1996 Jan;27(1):49-55.
To cite this abstract in AMA style:
Hayat S, Ballou S. A Retrospective Review and Prospective Intervention for Outpatient Follow-Up of Hospitalized Patients in Rheumatology [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/a-retrospective-review-and-prospective-intervention-for-outpatient-follow-up-of-hospitalized-patients-in-rheumatology/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-retrospective-review-and-prospective-intervention-for-outpatient-follow-up-of-hospitalized-patients-in-rheumatology/