Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
<
Background/Purpose: Connective tissue diseases such as scleroderma are frequently associated with interstitial lung disease (ILD). Detection of autoantibodies is crucial in characterizing disease phenotypes, but there remains a lack of substantial data on the association of some autoantibodies present in scleroderma patients with specific ILD patterns. We sought to investigate possible association, describe the phenotypes of scleroderma seen in our study cohort, and review findings from other studies.
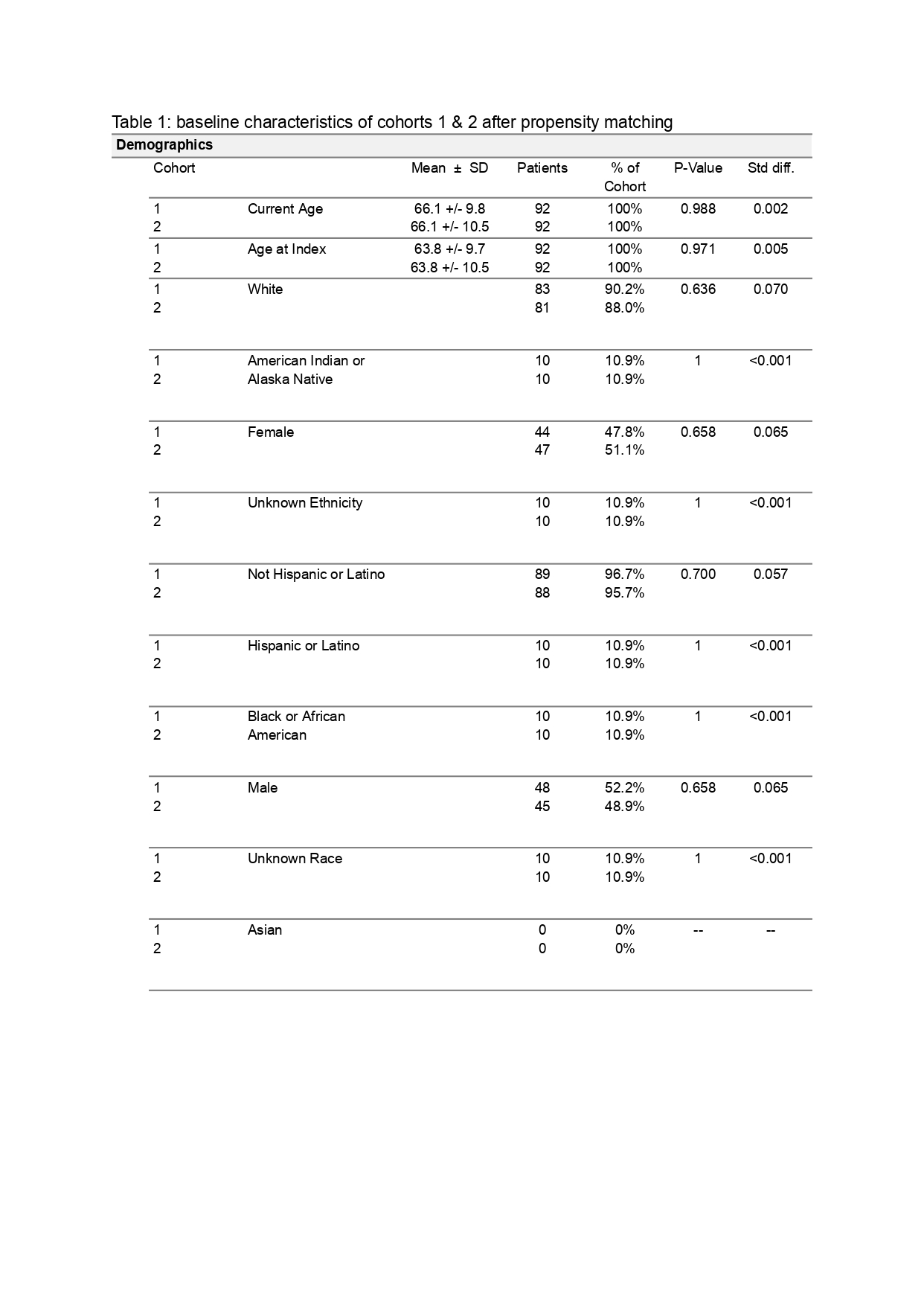
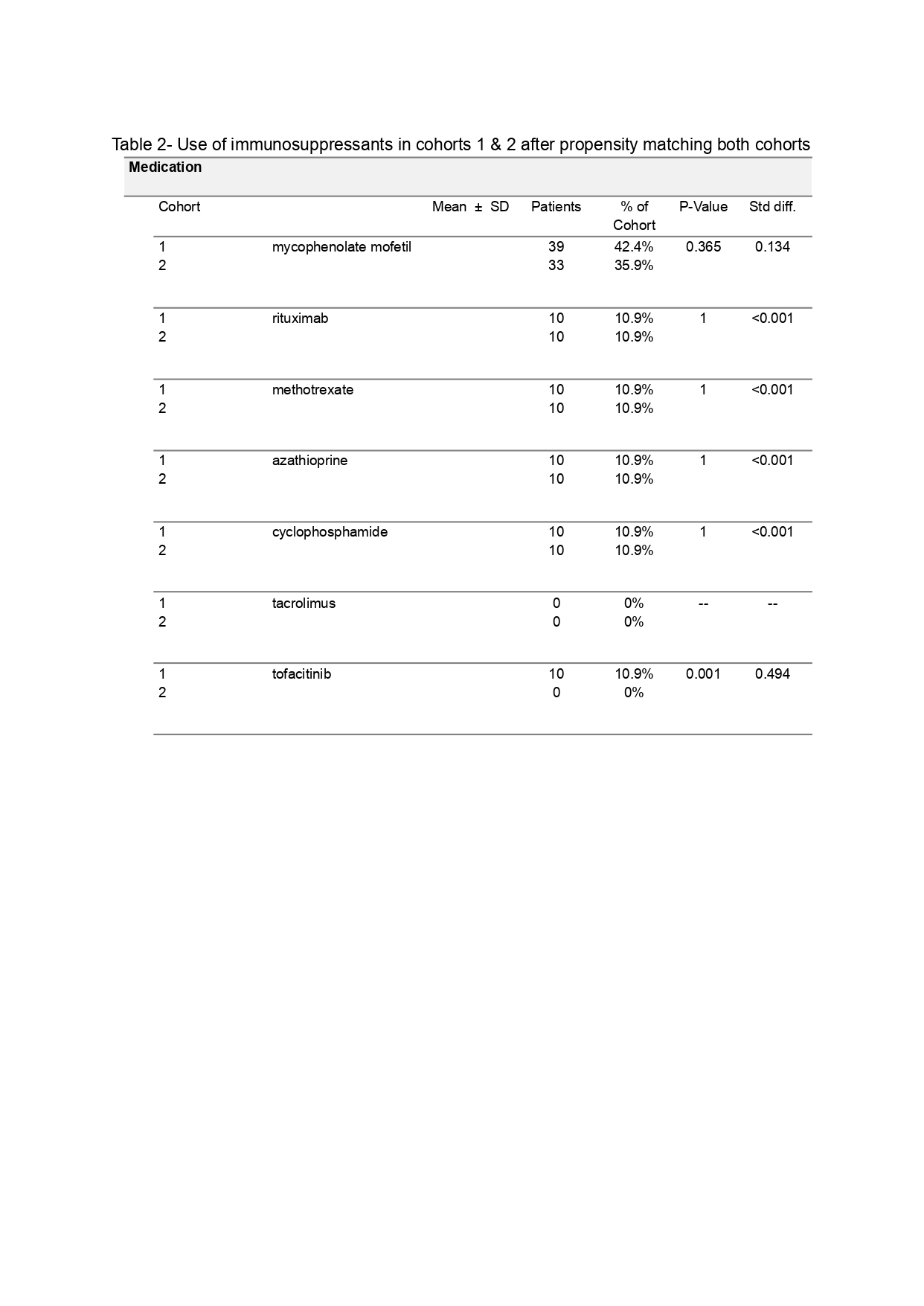
Methods: The cohort included adults with scleroderma and ILD who were treated at Mayo Clinic between January 2011 and December 2021. Baseline demographic, serologic, and imaging data were extracted from the electronic medical record. Continuous variables were summarized with median and range, and categorical variables were summarized with frequency and percentage (%). The Kruskal-Wallis Rank Sum test was used for continuous measures and the Chi-square test was used for categorical measures. All tests were two-sided and p-values less than 0.95 were considered to be statistically significant. Analysis programming was performed by R-studio with R version 4.1.2.
Results: A total of 454 patients with both scleroderma and ILD were included in the study. The study cohort had a mean age of 62 years, and 103 patients (22.7%) were males. ILD patterns analyzed included NSIP (83.3%), UIP (11%), probable UIP (2.9%), indefinite UIP (2.9%), OP (1.5%) and LIP (2%). The antibody and symptoms were determined for patients with and without each of these ILD patterns. NSIP patients were more likely to have anti-Scl70 antibodies compared to patients without NSIP ( p=0.01). OP patients were more likely to have anti-PM/Scl antibodies compared to patients without OP (p=0.006), and LIP patients were more likely to have anti-U1 snRNP antibodies compared to patients without LIP (p=0.002). LIP patients were significantly less likely to have antiScl70 antibodies than patients without LIP (p=0.025). Additionally, UIP patients were also less likely to have anti-Scl70 antibodies than patients without UIP (p=0.017). There were no clinically significant findings of anti-centromere antibodies or anti-RNA Pol III antibodies in any of the ILD patterns. No symptoms had a clinically significant association with the ILD pattern groups.
Conclusion: Our study examined associations between serologic data and ILD patterns and demonstrated a statistically significant association of anti-Scl70 antibodies with NSIP and antiPM/Scl antibodies with OP. There also appears to be an association between anti-U1 snRNP antibodies and LIP, which has not been demonstrated in the literature thus far aside from another observational study. LIP and UIP patterns were significantly less likely to have association with anti-Scl70 antibodies. We did not find any statistically significant association between anticentromere antibodies and specific ILD patterns. Finally, our study suggests that antibodies may develop in scleroderma but are not necessarily associated with development of ILD. Autoantibodies offer an invaluable tool in predicting disease outcomes and further studies are needed to elucidate this, especially with regards to scleroderma-associated ILD.
To cite this abstract in AMA style:
Uppal J, Vadlamudi K, Hasan S, Kattubadi A, Mishra M, Umer S, Hayat S, Muzaffar K. A Retrospective Analysis of the Efficacy of Nintedanib in Connective Tissue Disease-Associated Interstitial Lung Disease (CTD-ILD): A TriNetX Database Study [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/a-retrospective-analysis-of-the-efficacy-of-nintedanib-in-connective-tissue-disease-associated-interstitial-lung-disease-ctd-ild-a-trinetx-database-study/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-retrospective-analysis-of-the-efficacy-of-nintedanib-in-connective-tissue-disease-associated-interstitial-lung-disease-ctd-ild-a-trinetx-database-study/