Session Information
Title: Epidemiology and Public Health (ACR): Rheumatoid Arthritis and Systemic Lupus Erythematosus Outcomes
Session Type: Abstract Submissions (ACR)
Background/Purpose
Systemic lupus erythematosus (SLE) is a chronic, inflammatory disease which can impact on patients’ Health-Related Quality of Life (HRQoL). This analysis was designed to characterize US SLE patients classified by physicians as having “moderate-to-severe” disease, and to assess their burden of disease compared with those with “mild” disease severity.
Methods
Data were extracted from the multi-sponsor Adelphi 2013 Lupus Disease-Specific Program, a multinational survey of clinical practice. US physicians completed Patient Record Forms (PRFs); disease severity was based on physician assessments. Patients self-reported data including EQ-5D and Work Productivity and Activity Impairment Index for SLE (WPAI-Lupus), which were included in Patient Self-Completion Records (PSCs).
Results
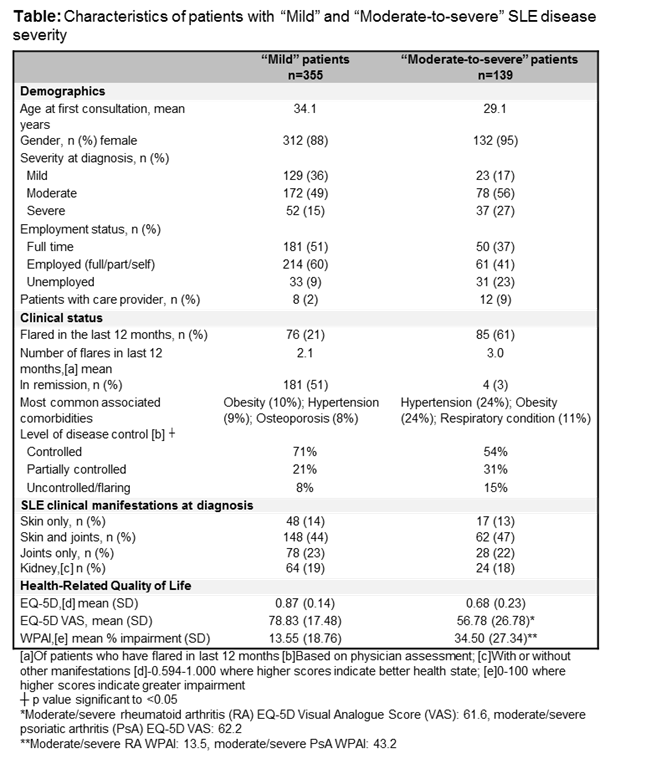
PRFs and PSCs were collected from 97 rheumatologists. Of 498 patients, disease severity was classified as “mild” in 355 (71%), and “moderate-to-severe” in 139 (28%) (severity was not specified in 4 patients [1%]). Physician assessment of disease severity was predominantly based on affected organs/symptoms (considered most important by 37% and 40% of rheumatologists, respectively). Only 11% reported test results/clinical assessments as a determinant of SLE severity, with no single disease activity index widely used in clinical practice; 68% rheumatologists reported using their own systematic assessment. Physician assessment of disease severity and control of disease activity were imperfectly correlated: disease activity was controlled in 54% of patients with “moderate-to-severe” disease severity, and partially controlled or uncontrolled in 29% of patients with “mild” disease severity. “Moderate-to-severe” patients initially presented with greater disease severity and organ involvement (13% had skin-only SLE at diagnosis), and more flares per 12 month period (Table), than “mild” patients. Compared to “mild” severity, “moderate-to-severe” SLE severity was associated with a greater impact on HRQoL, which was comparable to rheumatic conditions including rheumatoid arthritis and psoriatic arthritis (Table). Fewer “moderate-to-severe” patients were employed, and a higher proportion required care providers (Table). For both “mild” and “moderate-to-severe” patients, obesity was one of the most common associated comorbidities; the proportion of “moderate-to-severe” patients affected was over double that of “mild” patients (Table).
Conclusion
“Moderate-to-severe” SLE severity was associated with a greater burden of disease than patients with “mild” severity. Data show that disease severity is not consistently assessed in US clinical practice and is a multifaceted concept, imperfectly correlated with control of disease activity. Thus, there is a need for a simple, universal tool to accurately assess SLE disease activity, as well as severity, to inform physician and patient decisions regarding treatment.
Disclosure:
V. Strand,
AbbVie, Afferent, Amgen, Biogen Idec, Bioventus, BMS, Carbylan, Celgene, Celltrion, CORRONA, Crescendo, Genentech/Roche, GSK, Hospira, Iroko, Janssen, Lilly, Merck, Novartis, Pfizer, Regeneron, Sanofi, SKK, Takeda, UCB, Vertex,
5;
J. Johnson,
None;
C. Vandeloo,
UCB Pharma,
3;
C. Galateanu,
UCB Pharma,
3;
S. Lobosco,
None.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-real-world-characterization-of-us-patients-with-moderate-to-severe-systemic-lupus-erythematosus/